Antibody dependant enhancement of HIV leading to AIDS due to spike protein homology with glycoprotein 120?
Yes, it is in the transfection agents. Is it becoming clear yet what's happening?
…And made worse by combination with the much discussed VAIDS effects and selective pressure associated with higher viral loads.
Any extracts used in the following article are for non commercial research and educational purposes only and may be subject to copyright from their respective owners.
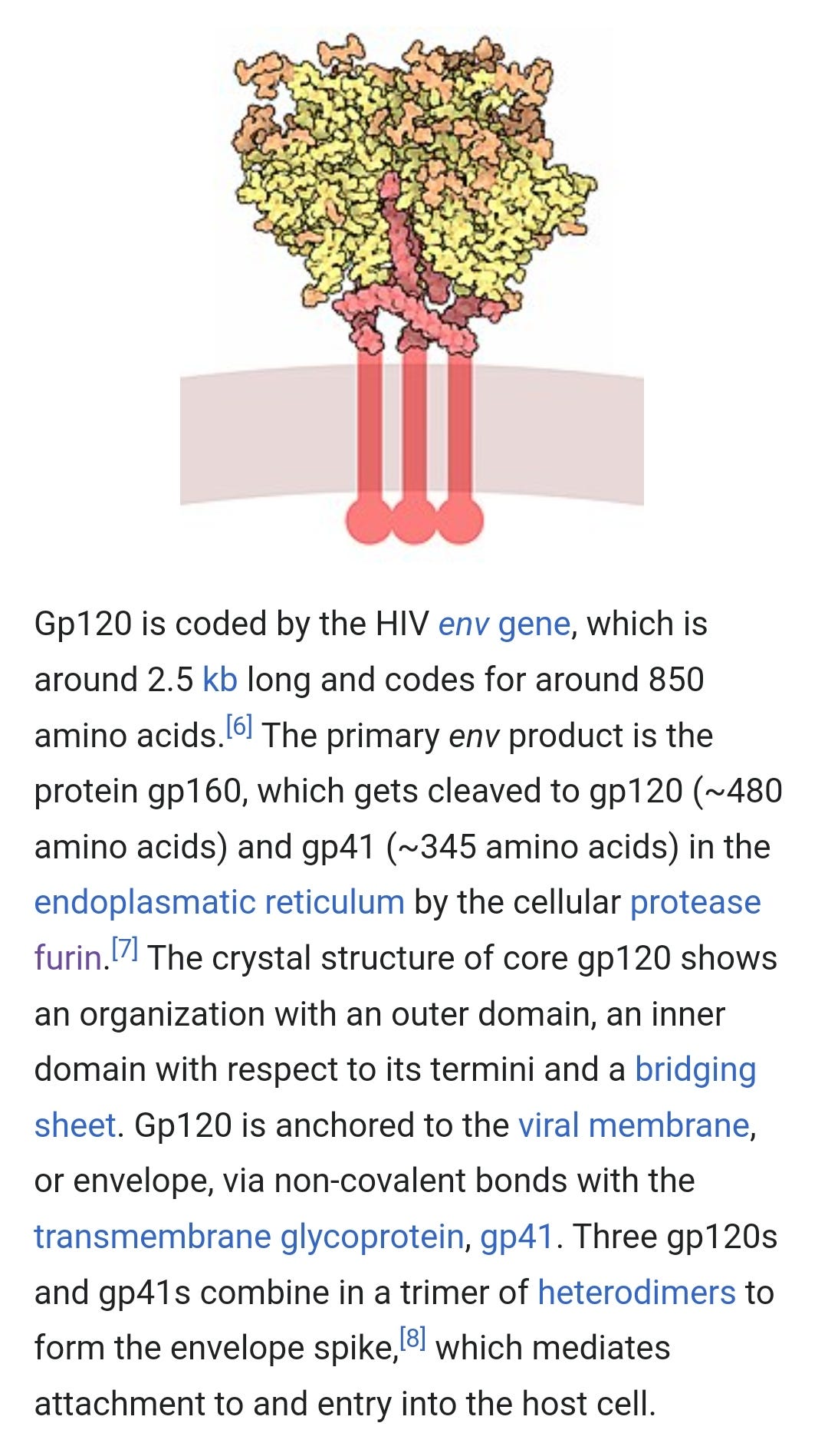
From Wikipedia:
“Unless a gp120-based vaccine can be designed to elicit antibodies with strongly neutralizing antiviral properties, there is concern that breakthrough infection leading to humoral production of high levels of non-neutralizing antibodies targeting the CD4 binding site of gp120 is associated with faster disease progression to AIDS.[21]”
https://en.m.wikipedia.org/wiki/Envelope_glycoprotein_GP120
The problem is the mirror of the following, the antibodies created to the homologous GP120 on the spike protein are equally cross reactive but non neutralizing with GP120 from HIV, and possibly disease enhancing as per the Wikipedia article:
Glycan reactive anti-HIV-1 antibodies bind the SARS-CoV-2 spike protein but do not block viral entry (2021)
Abstract
The SARS-CoV-2 spike glycoprotein is a focal point for vaccine immunogen and therapeutic antibody design, and also serves as a critical antigen in the evaluation of immune responses to COVID-19. A common feature amongst enveloped viruses such as SARS-CoV-2 and HIV-1 is the propensity for displaying host-derived glycans on entry spike proteins. Similarly displayed glycosylation motifs can serve as the basis for glyco-epitope mediated cross-reactivity by antibodies, which can have important implications on virus neutralization, antibody-dependent enhancement (ADE) of infection, and the interpretation of antibody titers in serological assays. From a panel of nine anti-HIV-1 gp120 reactive antibodies, we selected two (PGT126 and PGT128) that displayed high levels of cross-reactivity with the SARS-CoV-2 spike. We report that these antibodies are incapable of neutralizing pseudoviruses expressing SARS-CoV-2 spike proteins and are unlikely to mediate ADE via FcγRII receptor engagement. Nevertheless, ELISA and other immunoreactivity experiments demonstrate these antibodies are capable of binding the SARS-CoV-2 spike in a glycan-dependent manner. These results contribute to the growing literature surrounding SARS-CoV-2 S cross-reactivity, as we demonstrate the ability for cross-reactive antibodies to interfere in immunoassays.
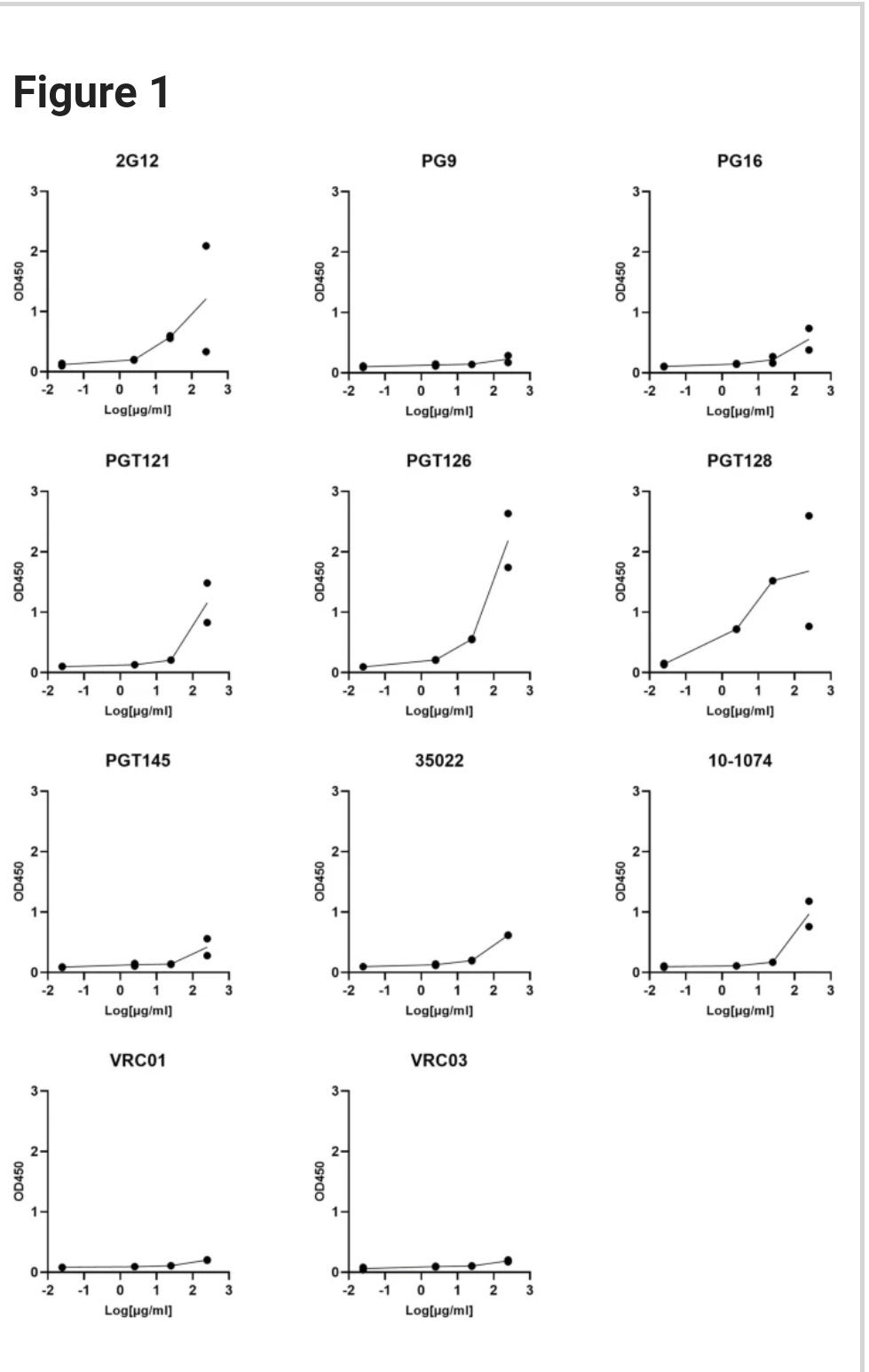
ELISA screen of glycan directed anti-gp120 antibody cross-reactivities to the SARS-CoV-2 Spike. Serial dilutions of the indicated mAbs were assessed for SARS-CoV-2 S protein binding. VRC01 and VRC03 target the CD4 binding site within gp120 and are included here as negative controls. All ELISAs were performed using BSA-based buffers (see methods). Experiments were done in duplicate and results are plotted as points.
https://www.nature.com/articles/s41598-021-91746-7
And this was withdrawn but the facts remain. You want non-neutralising antibodies, you've got them.
A shame the great Luc Montagnier is no longer with us.
Uncanny similarity of unique inserts in the 2019-nCoV spike protein to HIV-1 gp120 and Gag (2020)
Abstract
We are currently witnessing a major epidemic caused by the 2019 novel coronavirus (2019-nCoV). The evolution of 2019-nCoV remains elusive. We found 4 insertions in the spike glycoprotein (S) which are unique to the 2019-nCoV and are not present in other coronaviruses. Importantly, amino acid residues in all the 4 inserts have identity or similarity to those in the HIV-1 gp120 or HIV-1 Gag. Interestingly, despite the inserts being discontinuous on the primary amino acid sequence, 3D-modelling of the 2019-nCoV suggests that they converge to constitute the receptor binding site. The finding of 4 unique inserts in the 2019-nCoV, all of which have identity /similarity to amino acid residues in key structural proteins of HIV-1 is unlikely to be fortuitous in nature. This work provides yet unknown insights on 2019-nCoV and sheds light on the evolution and pathogenicity of this virus with important implications for diagnosis of this virus.
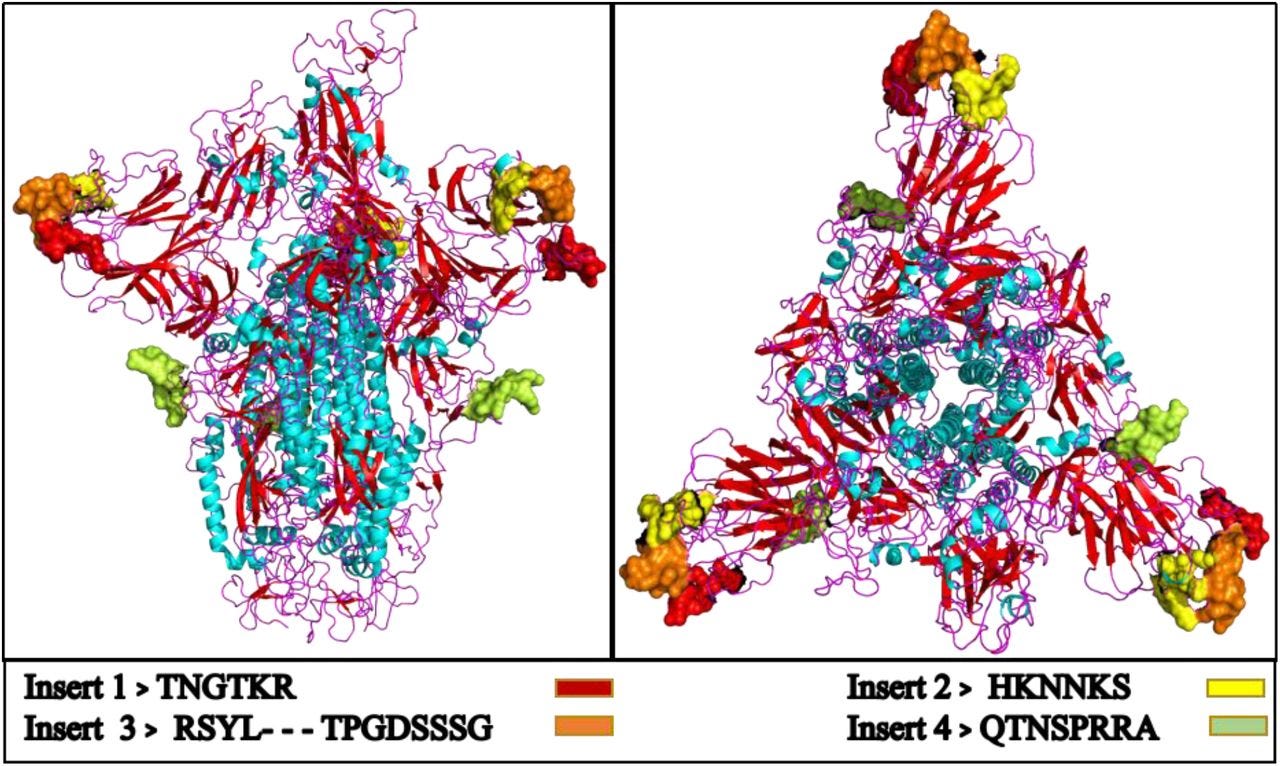
Figure 3.
Modelled homo-trimer spike glycoprotein of 2019-nCoV virus.
The inserts from HIV envelop protein are shown with colored beads, present at the binding site of the protein.
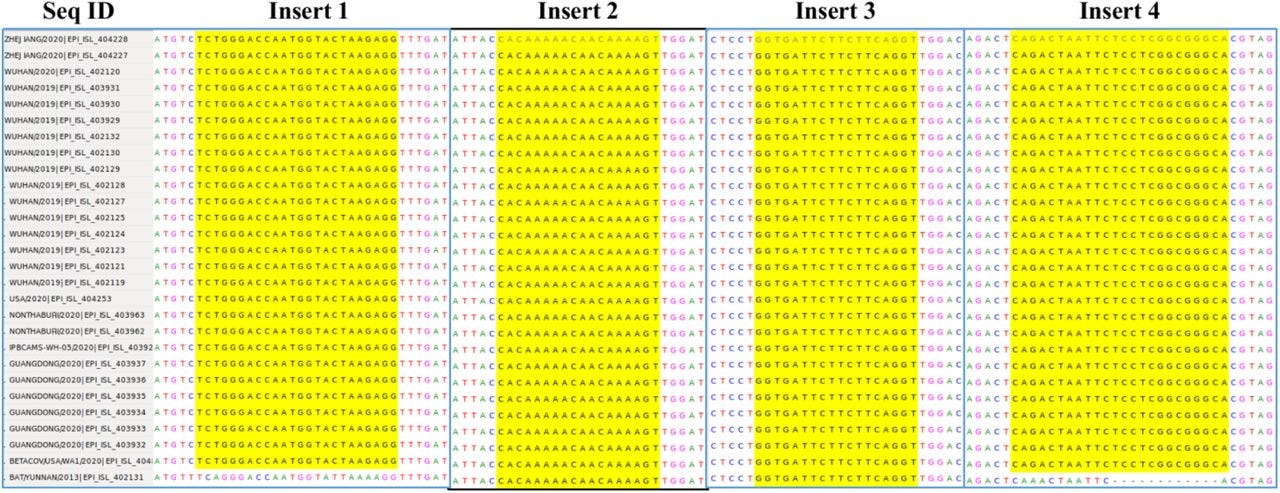
Fig.S2:
All four inserts are present in the aligned 28 Wuhan 2019-nCoV virus genomes obtained from GISAID. The gap in the Bat-SARS Like CoV in the last row shows that insert 1 and 4 is very unique to Wuhan 2019-nCoV.
https://www.biorxiv.org/content/10.1101/2020.01.30.927871v1
Further to the above, if you mis-prime your immune response around the mucosa you can unwittingly create vectors for transmission. Too much response is the problem, and something the naturally immune keep in check.
It's not looking good for a vax based solution, which is why it probably never worked well along with immune escape. And mRNA based snake oil is a loose cannon, as we know all too well.
You will almost never hear about natural immunity to HIV, it's a blasphemy and anathema to all things Pharma:
Natural Immunity to HIV: A Delicate Balance between Strength and Control (2012)
Abstract
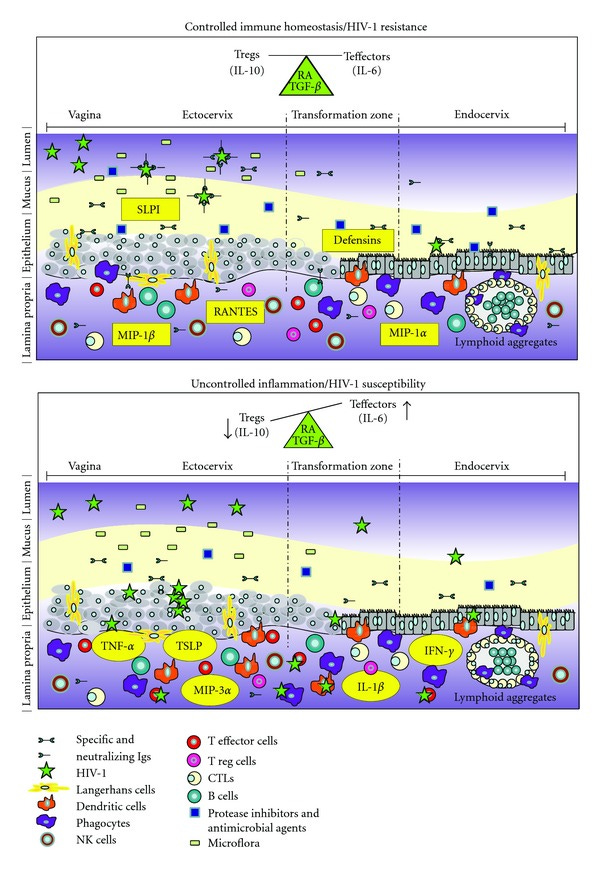
Understanding how the mucosal immune system in the human female reproductive tract might prevent or facilitate HIV infection has important implications for the design of effective interventions. We and others have established cohorts of highly-exposed, HIV-seronegative individuals, such as HIV-uninfected commercial sex workers, who have remained HIV-negative after more than 5 years of active prostitution. Observations obtained in studies of such individuals, who represent a model of natural immunity to HIV, indicate that HIV resistance may be associated with the host's capacity to preserve systemic integrity by constraining immune activity and controlling inflammatory conditions at the mucosal point of entry. This likely necessitates the orchestration of balanced, first-line and adaptive immune responses.
Qualitative and quantitative differences in mucosal innate and adaptive immune components are associated with the outcome of HIV infection in the female genital tract (FGT).
https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3529906/#__ffn_sectitle
Could certain COVID-19 vaccines leave people more vulnerable to the AIDS virus? (2020)
Cold-causing adenovirus used in four experimental COVID-19 vaccines increased risk of HIV infection when used in AIDS vaccine trials
Certain COVID-19 vaccine candidates could increase susceptibility to HIV, warns a group of researchers who in 2007 learned that an experimental HIV vaccine had raised in some people the risk for infection with the AIDS virus. These concerns have percolated in the background of the race for a vaccine to stem the coronavirus pandemic, but now the researchers have gone public with a "cautionary tale," in part because trials of those candidates may soon begin in locales that have pronounced HIV epidemics, such as South Africa.
Some approved and experimental vaccines have as a backbone a variety of adenoviruses, which can cause the common cold but are often harmless. The ill-fated HIV vaccine trial used an engineered strain known as adenovirus 5 (Ad5) to shuttle into the body the gene for the surface protein of the AIDS virus. In four candidate COVID-19 vaccines now in clinical trials in several countries, including the United States, Ad5 similarly serves as the "vector" to carry in the surface protein gene of SARS-CoV-2, the viral cause of the pandemic; two of these have advanced to large-scale, phase III efficacy studies in Russia and Pakistan.
In today's issue of The Lancet, four veteran researchers raise a warning flag about those COVID-19 vaccine candidates by recounting their experience running a placebo-controlled AIDS vaccine trial dubbed STEP. An interim analysis of STEP found that uncircumcised men who had been naturally infected with Ad5 before receiving the vaccine became especially vulnerable to the AIDS virus. The vaccine, made by Merck, had been the leading hope for what was then a 20-year search for a shot that could thwart HIV. But after the STEP results appeared, the field went into a tailspin. "It took a decade to recover," says one of the co-authors of the Lancet correspondence, Lawrence Corey of the Fred Hutchinson Cancer Research Center.
More:
EDITORIAL| VOLUME 28, ISSUE 11, P2303-2304, NOVEMBER 04, 2020
Pros and Cons of Adenovirus-Based SARS-CoV-2 Vaccines
Eric J. Kremer
October 09, 2020
"The origin of these effects likely lies in pre-existing anti-Ad immunity. Most adults have been infected by multiple Ad types and have persistent Ad infections. Together, this promotes long-lived anti-Ad B cell and T cell responses, include regulatory T cells (Tregs) that can dampen T cell responses. When injected with a bolus of Ad antigens (the vaccine), the response includes re-activation of anti-Ad effector memory T cells (TEMs), which return via homing receptors to the mucosal environments—where most Ad infections occur—and increased production of antibodies. Why are mucosal homing anti-Ad TEMs important? Some pathogens, like HIV, infect activated T cells in the mucosa.3 If you live in an environment where HIV acquisition is a risk, then the last thing you want to do is provide HIV with an easy target. Increased HIV spread will fall below the radar of vaccine safety criteria because it is typically not included as an endpoint measurement."
"Most data suggest that the immune response to coronavirus is transient (<6 months).4 With regard to COVID-19, the more severe the clinical complications, the greater the immune response against SAR-CoV-2, as is the case for most viral infections. Therefore, asymptomatic/mild COVID-19 would induce a lower immune response that would disappear within weeks. Fold this onto the kinetics and efficacy of an Ad-based vaccine, and the law of parsimony suggests that we need long-term antigen expression in a favorable environment to generate long-term protection. Yet, in ∼70% of us our anti-Ad TEMs will target vaccine-infected cells. Is it possible that Ad-specific Tregs could prevent lysis of vaccine-infected cells and allow long-term expression of SARS-CoV-2 antigens? This would be a welcome surprise. Follow-up studies from HIV and Ebola Ad-based vaccines suggest that a 4-dose vaccine regimen can induce immune hallmarks of protection for up 2 years. But the idea of 4 doses/person for billions of people during the first round of vaccinations—perhaps followed by booster shots every year—is difficult to imagine. While at least one phase 1 trial suggested that a 1-shot Ad-based vaccine could be sufficient, it is probable that this will be transient protection in most adults and particularly ephemeral protection in seniors."
More: