Neurological disorders and autoimmune diseases: A new perspective
When the abnormal looks normal
Reading time:
short story - novelette - novella - novel - PhD thesis - Trump’s tariff list - War and Peace - U.S. Tax Code
TL;DR: A study from 2023 discussed how autoimmune dysfunction may underlie some syndromes such as chronic fatigue syndrome (ME/CFS) or fibromyalgia syndrome (FMS), yet your lab test results test normal for pathogenic and natural autoantibodies (AAb). This is one of the reasons why progress in developing diagnostic techniques and treatments has stalled.
Any extracts used in the following article are for non-commercial research and educational purposes only and may be subject to copyright from their respective owners.
Contents
Introduction
Every so often, you will come across a research paper that breaks new ground, at least from my perspective, and makes you look at what you thought you knew in a different way.
One such paper was published in 2023, and I will walk you through it later.
Due to molecular mimicry and disruption of the function of regulatory T cells (Tregs) experimental gene therapy SARS-CoV-2 mRNA/LNP agents are responsible for inducing a wide range of autoimmune disorders in susceptible individuals. Perhaps it’s a new-onset condition, a relapse, or it leads to rapid progression of an existing condition.
This was predicted in advance by scientists such as Dr James Lyons-Weiler, and I discussed some of the mechanisms and autoimmune antibodies previously. Bio-engineered spike protein is pathogenic regardless of source: viral or engineered.
Homology between human and viral proteins is an established factor in viral- or vaccine-induced autoimmunity. Failure of SARS and MERS vaccines in animal trials involved pathogenesis consistent with an immunological priming that could involve autoimmunity in lung tissues due to previous exposure to the SARS and MERS spike protein.
Exposure pathogenesis to SARS-CoV-2 in COVID-19 likely will lead to similar outcomes. Immunogenic peptides in viruses or bacteria that match human proteins are good candidates for pathogenic priming peptides (similar to the more diffuse idea of "immune enhancement").
Here I provide an assessment of potential for human pathogenesis via autoimmunity via exposure, via infection or injection.
SAR-CoV-2 spike proteins, and all other SARS-CoV-2 proteins, immunogenic epitopes in each SARS-CoV-2 protein were compared to human proteins in search of high local homologous matching. Only one immunogenic epitope in a SARS-CoV-2 had no homology to human proteins.
From: “Pathogenic priming likely contributes to serious and critical illness and mortality in COVID-19 via autoimmunity“ (Apr ‘2020)
This Substack is a follow-up to the post from 25th November ‘23.
A Hat tip to Walter for this recent post. He discusses clinical evidence to support what resembles pathogenic priming: an autoimmune condition, APS, that follows a second infection or repeated boosters:
Discussion
Gaslighting by the NHS
By now, almost five years after their rollout, most of us know of someone who has developed neurological symptoms that they cannot readily explain. They may put it down to age, stress, lack of sleep, poor diet, COVID-19, or something else.
Eventually, it’s severe enough to prompt a visit to their GP, and the GP adds them to the waiting list to see a specialist for diagnosis.
It might be something like this:
However, despite repeated tests and being passed around for several months, the cause remains undiagnosed.
It’s useful at this point to define the following:
Clinical sign: “something found during a physical exam or as a result of a laboratory or imaging test that shows that a person may have a condition or disease. Signs can be observed by a health care provider or other person.”1
Condition: “In medicine, a term that refers to a person's state of health. For example, a patient's condition in the hospital may be described as good, stable, or serious. Condition may also refer to a normal state with regard to one's health, such as pregnancy, or to a disease, disorder, illness, or injury.”2
Symptom: “Something that a person feels or experiences that may indicate that they have a disease or condition. Symptoms can only be reported by the person experiencing them. They cannot be observed by a health care provider or other person and do not show up on medical tests. Some examples of symptoms are pain, nausea, fatigue, and anxiety.”3
Syndrome: “A set of symptoms or conditions that occur together and suggest the presence of a certain disease or an increased chance of developing the disease.”4
Disorder: “In medicine, an abnormal condition that affects the body's function but may or may not have specific signs and symptoms. A disorder may indicate that a specific disease is present, but there is usually not enough evidence to make a diagnosis. There are many different types of disorders, including physical, mental, emotional, behavioral, genetic, and functional disorders.”5
Disease: “An abnormal condition that affects the structure or function of part or all of the body and is usually associated with specific signs and symptoms.”6
The catch-all non-diagnosis at the end of the line may be that you are suffering from a Functional Neurological Disorder (FND), rather than the true cause, which in many cases is due to vaccine poisoning:
“The Rehab Team” in New Zealand summarised seven myths surrounding FND7.
There is a reason why these myths arose in the first place, and its because it is, or was, cultural within allopathic medicine. If it wasn’t then these “misinterpretations” wouldn’t have arisen in the first place. They would have quickly been quashed due to the patient’s positive experience or due to advice from a qualified medical professional:
Myth One: FND is a diagnosis of exclusion.
Diagnosis of FND should be approached in the same way as any other condition and be diagnosed based on positive clinical findings like the Hoover test and entrainment test.
Myth Two: Patients have either FND or another Neurological Condition.
Different neurological conditions can occur together. FND can commonly occur with other neurological conditions at the same time.
Myth Three: FND is all in your head
FND is absolutely NOT “faking” or made up symptoms. Functional MRI studies show it is a very real disorder that occurs due to a very real brain/body disconnect.
Myth Four: FND symptoms are voluntary
FND symptoms are involuntary and are out of the direct control of the person experiencing the. This can be terrifying. It is not possible for people with FND to “get over their symptoms” or “snap out of it”.
Myth Five: There is less harm in missing a diagnosis of FND than missing other Neurological Conditions
Any misdiagnosis is distressing but missing a diagnosis of FND, a potentially treatable condition, compared to any other neurological condition can be as harmful as the reverse occurring.
So, it is mainly “a psychological condition” then?
Myth Six: FND is exclusively a psychological problem.
FND is a complex interaction of psychological, physical , sensory, motor control, lifestyle and autonomic influences. FND is not solely a psychological condition.
Myth Seven: You can’t get better if you have FND.
There is HOPE. Most people who engage in FND specific treatment with a provider who understands FND and specific FND treatment approaches find they have improvement in their symptoms. Just like any neurological condition, there is a spectrum of disease severity so the level of improvement with rehabilitation will vary. Some will recover and some will have long term symptoms, especially if left untreated.
Functional Neurological Disorder (FND) is a common condition. A clear diagnosis provided in a timely manner can have a strong positive impact on improvement of symptoms. Everyone diagnosed with FND should be referred for treatment and rehabilitation. If this is not the case, it is important to find your own FND provider to get the support you need.
As autoimmune neurological disorders exist on a spectrum of overlapping autoAbs and symptoms, then you may be misdiagnosed with a disease that fits closest to your signs, symptoms and clinical tests.
The problem with being misdiagnosed with FND or another disease is that you may receive the wrong treatment, so that a cure is unlikely, or they may just be treating your symptoms. This puts you at risk of side effects or complicates the use of other drugs.
Fibromyalgia
Also called fibromyalgia syndrome (FMS), it’s a long-term condition that causes pain all over the body.
From the relevant NHS website.8
(Emphasis in bold is mine):
Symptoms of fibromyalgia
As well as widespread pain, other symptoms of fibromyalgia include:
increased sensitivity to pain
muscle stiffness
difficulty getting to sleep or staying asleep, which can make you feel very tired (fatigue)
problems with mental processes (known as "fibro-fog"), such as difficulty concentrating or remembering things
irritable bowel syndrome (IBS), a digestive condition that causes stomach pain and bloating
feelings of frustration, worry or low mood
The symptoms of fibromyalgia are changeable – for example, they can sometimes suddenly improve or get worse.
See a GP if you think you have fibromyalgia. Treatment can ease some of the symptoms, although they're unlikely to disappear completely.
How fibromyalgia is treated
Although there's currently no cure for fibromyalgia, there are treatments to help relieve some of the symptoms and make the condition easier to live with.
Treatment tends to be a combination of:
lifestyle changes, such as exercise programmes and relaxation techniques
talking therapies, such as cognitive behavioural therapy (CBT) and acceptance and commitment therapy (ACT)
medicine, such as antidepressants
In particular, exercise has a number of important benefits for people with fibromyalgia, including helping to reduce pain.
What causes fibromyalgia?
The exact cause of fibromyalgia is unknown, but it's thought to be related to abnormal levels of certain chemicals in the brain and changes in the way the central nervous system (the brain, spinal cord and nerves) processes pain messages carried around the body.
It's also suggested that some people are more likely to develop fibromyalgia because of genes inherited from their parents.
In many cases, the condition appears to be triggered by things that are physical or emotional like an injury, an infection or stress.
I’ve linked to this before, and unfortunately the website isn’t due to be reviewed until 12th October ‘25.
Hopefully by then the NHS will at least consider the many research papers discussing the contribution of autoimmune dysfunction, as well as at least mention the existence of alternative therapeutics.
But I wouldn't bank on it, the market for drugs and quack treatments that only address symptoms is far too lucrative:
Based on market forecasts, the fibromyalgia treatment sector will expand from USD 2.89 billion in 2024 to USD 4.40 billion by 2034, experiencing a CAGR of 4.3%. The rising demand for Fibromyalgia treatment is driving market growth, with innovative therapies emerging. In 2023, medications led with a 68% market share, while retail pharmacies dominated distribution at 54%. North America was the top contributor, holding 40% of the market.
Fibromyalgia tends to increase with age. Between 20 to 55 years old, it's often the main reason for widespread muscle pain in women. Teenagers can also have fibromyalgia at similar rates to adults. And in specialized pain clinics, over 40% of patients meet the criteria for fibromyalgia.
If someone already has a rheumatic disease, they have a higher chance of getting fibromyalgia. Doctors suggest using both non-drug treatments and medications for most fibromyalgia patients. Some people might find relief with non-drug treatments alone. Certain antidepressants and anticonvulsants have been shown to help with fibromyalgia pain. These include drugs like amitriptyline, duloxetine, and pregabalin. The US FDA has approved pregabalin, duloxetine, and milnacipran specifically for treating fibromyalgia. Therapy usually starts with antidepressants. If those don't work well, an anticonvulsant or another type of antidepressant may be tried. In more severe cases where fatigue, depression, or sleep problems are very bad, an anticonvulsant or a different antidepressant might be recommended.
An online survey was conducted among university students across various universities in Egypt. This study aimed to explore the prevalence and factors contributing to fibromyalgia among students, as well as it is influence on their quality of life-related to health.
Wrongly Diagnosing a Condition Can be Hard on Patients Emotionally
Misdiagnosis happens when doctors mistake one condition for another. With fibromyalgia, this can be a big problem because of this, many people with fibromyalgia don’t get the right diagnosis at 1st. they might go through a long process of trying different treatments for conditions they don’t have, which can be frustrating and tiring.
For instance,
Someone with fibromyalgia might have widespread pain, fatigue, and trouble sleeping, which are symptoms of other conditions. So, doctors might 1st think its something else and try treatment for those conditions. But if those treatments don’t work, or if the symptoms get worse, they might consider fibromyalgia as a possibility later on.
Almost 40% of the 1,000 respondents in the UK survey were unaware of fibromyalgia, and another 23% were unsure if they knew what it was. This is in line with the rising number of searches for the condition over time.
From: “Fibromyalgia Treatment Market Size, Key Players & Emerging Therapies“
https://www.towardshealthcare.com/insights/fibromyalgia-treatment-market-sizing
Interesting observations about reported FMS prevalence at university. This requires further investigation or explanation.
A review paper from 2023 by McConnell et al. provides some useful statistics and recommendations to GPs. This may be useful information for any readers who have been diagnosed, or know someone who is.
Key takes from “Explaining a diagnosis of fibromyalgia in primary care: a scoping review“9:
Background Fibromyalgia is a common cause of chronic pain in the UK, with a huge individual and societal impact. Despite this, it remains difficult to diagnose and treat. The explanation of a fibromyalgia diagnosis can lead to difficult therapeutic relationships, with attitudinal issues and negative profiling of patients. This can lead to frustration, and have a harmful impact on health outcomes.
Aim To review how an explanation of a fibromyalgia diagnosis is provided in primary care in order to establish a model of best practice when educating patients on their diagnosis.
Design & setting Scoping review of articles written in English.
Method MEDLINE, Embase, Web of Science, and grey literature were searched. Articles were extracted, reviewed, and analysed according to the inclusion criteria.
Results In total, 29 records met the inclusion criteria. The following six overarching themes were identified: patient education; physician education; importance of the multidisciplinary team; importance of patient-centred care; the value of primary care; and useful resources. The literature illustrated that describing fibromyalgia using analogies to illustrate the pain sensitisation process can help patients understand their diagnosis better. This improves their willingness to accept management plans, particularly engagement with non-pharmacological therapies, which the literature suggested are best delivered within a multidisciplinary team.
Conclusion Key aspects of fibromyalgia should be explained to patients in order for them to gain a better understanding of their diagnosis. A 'one-size-fits-all' model for explaining the fibromyalgia diagnosis to patients is inappropriate because patients' experiences are individualised. Further research is required on whether different explanations impact patient outcomes.
Your case may not even reach the desk of a specialist:
How this fits in
The GP has a vital role in the management of chronic disease, including chronic pain. Fibromyalgia is one of the most common causes of chronic pain in the UK yet often results in difficult therapeutic relationships, with attitudinal issues and negative profiling of patients. As fibromyalgia is increasingly managed within general practice, it is vital that patients are provided with an adequate explanation of their diagnosis in order to improve consultations for both the patient and physician.
It’s a huge problem:
Chronic pain has a high prevalence across global populations. The Global Burden of Disease Study 2016 affirms this, with pain and pain-related diseases being the leading cause of disability and disease burden.1
Here in the UK, there have been multiple publications that quote a wide range for the prevalence of chronic pain. In a systematic review encompassing UK-based studies, a pooled estimate of chronic pain prevalence was reported at 43.5% for the general population.2
In the Health Survey for England 2017, it was estimated that approximately 15.5 million people in England have chronic pain, with nearly one-third of these suffering from high-impact chronic pain, to an extent that it affects their activities of daily living such as self-care and ability to work.3
Fibromyalgia is one of the most common causes of chronic pain in the UK, with a huge individual and societal impact.
While global prevalence is estimated between 2% and 6%, the UK prevalence is estimated at 5.4% of the general population.4 Despite this, fibromyalgia remains difficult to treat.
This is far from satisfactory, although I can understand why:
No single treatment works for every symptom or for every patient, and the aim of treatment is to improve quality of life while living with pain, as opposed to curing the pain.5,6
In 2021, the National Institute for Health and Care Excellence (NICE) updated its guidance on the treatment of chronic pain in adults, including fibromyalgia.6 It recommends performing a person-centred assessment, enabling patients to actively participate in their care, and exploring how their pain affects their daily life.
It’s good to see guidance moving away from painkillers, but as we shall see in the headline paper, this also risks dismissing therapeutics that may address some of the root causes. Traditional Chinese Medicine (TCM) takes a more holistic approach, for example:
Furthermore, it advises developing a care and support plan in conjunction with the patient, exploring their capabilities and goals. NICE also advises the use of non-pharmacological methods to manage pain, including supervised exercise programmes and psychological therapies.6,7
While guidelines are available for the diagnosis and management of fibromyalgia, unfortunately it remains a difficult concept for patients and clinicians to grasp, with the literature suggesting that it can be a frustrating condition for both patients and healthcare professionals, often resulting in difficult therapeutic relationships.8–11 Additionally, the communication of a fibromyalgia diagnosis is recognised to be of vital importance to aid the recommended treatment modalities, such as psychological therapy, supervised exercise programmes, and other non-pharmacological options.5,12
Importance of the multidisciplinary team
As fibromyalgia has a multitude of symptoms, including widespread pain, fatigue, cognitive symptoms, and sleep disturbance, a multimodal treatment strategy is recommended.5,37
This multimodal treatment strategy included patient education, pharmacotherapy, and non-pharmacotherapies, comprising exercise, cognitive behavioural therapy, and sleep hygiene. As a result, cooperation between multiple different healthcare professionals including doctors, nurses, physiotherapists, and psychologists is recommended.5,26
Furthermore, consistent communication to patients regarding chronic widespread pain is encouraged between the different members of the multidisciplinary team, from primary to specialist care, to avoid confusion and conflicting messages.37
More: https://bjgpopen.org/content/7/4/BJGPO.2023.0033
The temporal association between vaccine administration and onset of symptoms, coupled with my understanding of the mechanisms of autoimmune dysfunction, strongly leads me to suspect that autoAbs are at the core of many neurological disorders.
In January 2024, Clauw et al. addressed the issue in “Is fibromyalgia an autoimmune disorder?”10.
They asked two experts with opposing views to discuss the evidence for and against.
Highlights
Certain aspects of FM are still controversial, including pathophysiology, which remain a subject of debate
FM shares many clinical features, sometimes designing overlapping diseases, with other conditions, including, chronic fatigue syndrome (CFS), sick building syndrome (SBS), post-COVID syndrome, and many others
Anti-GPCR (anti- G protein-coupled receptor antibodies), autoantibodies directed against the autonomic nervous system receptors, have been detected in the serum of patients with FM, and their titers correlated with clinical symptoms
Fibromyalgia belongs to nociplastic pain which means that the central nervous system is the driving force behind this pain mechanism, and the key phenotypic features include widespread pain, fatigue, and sleep, memory, and mood disturbances
Abstract
Fibromyalgia (FM) is a multifactorial syndrome which includes not only widespread pain and stiffness, now recognized as major symptoms, but also numerous other somatic, emotional, and neuropsychic manifestation.
The lack of specific validated biological and instrumental biomarkers has made FM a condition of unexplained medical significance, and its pathophysiology remains controversial and subject to debate.
The current hypothesis regarding the pathogenesis of FM proposes that its development is influenced by various mechanism, including genetic predisposition, stressful life events, inflammatory processes, and cognitive-emotional factors. However, despite the extensive research conducted to date, the available data do not provide a clear understanding of the pathogenesis of FM.
There is a definition for FMS based on pain alone:
Fibromyalgia (FM) is a multifactorial syndrome characterized by chronic widespread pain (CWP), as defined by the International Association for the Study of Pain (IASP) as “pain in at least 4 of 5 body regions (in at least 3 or 4 body quadrants)” [1,2].
As per the market analysis discussion, it is associated with other disorders:
It primarily affects women during their fifth decade of life, but it can occur at any age and may be associated with various conditions, including chronic fatigue syndrome, anxiety, irritable bowel syndrome, and most of musculoskeletal rheumatic diseases [5].
There is no single known marker that can confirm a diagnosis:
Certain aspects of FM are still controversial, including pathophysiology, which remain a subject of debate. Specifically, the lack of specific validate biological and instrumental biomarkers has made FM an emblematic condition of unexplained medical significance, and still many physicians, in agreement with Perrot's 2012 statement, continue to express doubts about its entity [6,7].
I fully agree with these sentiments:
Nonetheless, due to the high prevalence of the disease and its significant impact on the lives of affected patients, it is essential for the scientific community to make a concerted effort to better define the aspects, especially pathophysiological one, that characterize this condition [8].
The biopsychosocial model of FMS:
… it constitutes an integrated pattern of neuro-inflammatory and psycho-social factors, with a dynamic interaction between them.
Genes and stress? This sounds like something of a cop-out. I’m not saying they don’t contribute to the syndrome, but that they aren’t the root cause. Otherwise, why don’t we all suffer from FMS? What is missing in the “healthy”?
This model would be the basis for the current pathogenetic hypothesis, which suggests that FM develops due to the interplay between various mechanisms, including genetic predisposition, stressful life events, inflammatory, and cognitive-emotional factors.
This combination can result in neuromorphological changes, included a hyper-activation of brain areas dedicated to pain, as well as a reduction in the endogenous pain inhibitory signal [15,16], that lead to the onset of nociplastic pain and altered pain perception, commonly observed in FM patients.
This is more in line with the observed pathologies, especially considering what we know about magnesium deficiency and FMS:
Studies have shown that altered levels of pro-inflammatory cytokines (such as interferon-γ, interleukine (IL)-5, IL-6, IL-8) lead to chronic low-grade inflammation [18], which sensitizes neurons at all levels of the pain transmission chain, making them more excitable. Subsequently, it results in the activation of the innate and adaptive immune systems, leading to the secretion of cytokines, inflammatory and neuro-sensitizing molecules, which can dysregulate the complex nociceptive system.
Talking of pain:
… Magnesium is known to play an important role in the prevention of central sensitization by blocking N-methyl-D-aspartate (NMDA) receptors in a voltage-dependent manner.11 Magnesium deficiency has been largely associated with muscle pain along with fatigue, sleep difficulties, and anxiety; all of which are common symptoms of fibromyalgia.12,13 In some studies, it is thought that magnesium deficiency, through reductions in muscle ATP levels, may play a role in the development of fibromyalgia.14 Other studies correlate increased levels of substance P (a neurotransmitter known for its role in pain perception) with magnesium deficiency as well as pain intensity in fibromyalgia, raising the question of a possible correlation between magnesium deficiency and fibromyalgia.15-17
From: “Magnesium and Fibromyalgia: A Literature Review“ (2021)
Also see:
It has been reported that patients with FM in some cases showed a small fibers neuropathy (SFN). It is a condition that affects the small nerve fibers in the skin and other organs. These fibers are responsible for transmitting sensory information such as pain, temperature and touch [19].
Moreover, this condition has been induced in mouse models by the transfer of sera rich in anti-GPCR antibodies [20,21]. When SFN occurs, the affected nerve fibers are damaged or destroyed, resulting in a wide range of symptoms [22]. This includes symptoms such as dysesthesia, burning pain, and autonomic dysfunction [23,24], which are commonly observed in patients with FM.
The link between dysbiosis and disease is one that frequently appears in the literature, and we discussed it in a couple of recent review papers:
“Interplay between Multisystem Inflammatory Syndrome in Children, Interleukin 6, Microbiome, and Gut Barrier Integrity”11
and:
“Could the Spike Protein Derived from mRNA Vaccines Negatively Impact Beneficial Bacteria in the Gut?”12
Also see this Substack:
The gut-brain axis (GBA) links dysbiosis to neurological disorders13. Kefir anyone?
Some papers have reported that individuals with FM have alteration in gut microbiota composition and function, which may contribute to the development of chronic pain and other symptoms [28,29].
These changes in gut microbiota may results in increased intestinal permeability (also known as “leaky gut”), which allows harmful substances to enter the bloodstream and trigger an immune response [29].
In addition, alterations in the gut-brain axis may also affect the production of neurotrasmitters such as serotonin and dopamine, which play a role in pain modulation and mood regulation.
Dysregulation of these neurotransmitters may contribute to the development of FM symptoms [30].
Arguments in support of the hypothesis that FM is an autoimmune disease, by Professor Yehuda Shoenfeld:
(CWS: Chest wall syndrome - chest pain without an obvious cause, such as acute coronary syndrome or a pulmonary embolism14).
FM is a clinical condition characterized by a panoply of symptoms such as CWS, fatigue, paresthesia, cognitive impairment, sleep disturbances, memory loss, as well as dryness of mouth and eyes, hearing loss, tachycardia, and many others [24,[31], [32], [33]].
Despite extensive testing, there is currently no conceivable pathophysiological explanation for all these subjective complaints [23,31]. FM shares many clinical features, sometimes designing overlapping diseases, with other conditions, including, chronic fatigue syndrome (CFS) [34], sick building syndrome (SBS) [35], post-COVID syndrome [36,37], and many others [23,24,31,32,38].
We return to this paradox later:
Patients complaining of these overlapping clinical conditions get subjected to many instrumental examinations, and extensive blood work, which are often result in clinical pictures in the normal range.
This is where the gaslighting comes into the equation. And there we have it. The NHS consider you to be healthy, and sends you away with the equivalent of a sugar pill:
Patients are consequently considered healthy and are prescribed anti-depressant or anti-anxiolytic drugs, considering the symptoms merely functional [24,31,39].
“Myths” you say? Note the use of “functional”, as in FND.
We need to drag the NHS and other bodies away from nineteenth-century quack medicine:
Among the most supportive evidence that FM may be an autoimmune disorder are anti- G protein-coupled receptor (GPCR) antibodies (Ab) and the Small Fiber Neuropathy (SFN).
Anti-GPCR, autoantibodies directed against the autonomic nervous system receptors [23,32,33,40], have been detected in the serum of patients with FM, and their titers correlated with clinical symptoms [39].
The autoantibodies have also been found in patients with the other clinical conditions that overlap with FM [24,31,33].
According to the Ernst Witebsky and Noel Rose's criteria for autoimmune disease diagnosis, a passive transfer of these autoantobodies should induce all the clinical symptoms in experimental models [41,42].
The transfer of FM patients's Immunoglobuline G had led to all the clinical findings in mice, including the development of a SFN [20,21]. In addition, sera of subjects with FM in which anti-GPCR autoantibodies were extracted, transferred to mice, did not result in the development of clinical manifestation [32,43].
SFN was also found in all the clinical overlapping conditions, including fibromyalgia; and may explain several additional many of the clinical manifestations reported by the patients, i.e. paresthesiae, widespread pain, severe fatigue [37,44,45].
Only when you are honest about potential causes can you be serious about treating it successfully:
The fact that fibromyalgia is an autoimmune disease induced by anti-GPCR autoantibodies also has clinical therapeutical implications – plasmapheresis with IVIG (intravenous high dose gammaglobulin) infusion may have beneficial effects on the subjects.
These beneficial effects are supplementary to therapy with progressive exercise. The positive results were described in all the clinical overlapping conditions in which dysautonomia can be detected [20,34,46,47]. The improvement effects of exercise in these conditions stems from stabilizing of the para-sympathetic arm of the autonomous nervous system [48,49].
Arguments against the hypothesis that FM is an autoimmune disease, by Professor Daniel Clauw.
(Note that both Profs. Clauw & Shoenfeld were co-authors of this paper):
Asserting that FM is an autoimmune disease is incorrect.
Until recently most research into FM had been performed by rheumatologists, who are clinically trained to diagnose and treat autoimmune disorders. The rheumatologists studying this condition, as well as their peers in practice, agreed that FM was much different clinically than the autoimmune disorders that they were seeing in practice.
IgG4-related disease (IgG4-RD) is also an immune-mediated disorder. Yet as IgG4 is an antibody with anti-inflammatory properties it would be incorrect to make this a disqualifying criterion.
Your move.
In light of the fact that there was no inflammation identifiable in these individuals, either on examination or in laboratory testing, the name of the condition was even formally changed from fibrositis to fibromyalgia in the 1970's [50].
At this point in time, even though many rheumatologists were not certain FM was a real disease, they were quite certain what it was not – an autoimmune disease [7]. This remains the case today.
Much like their approach to another elephant in the room:
Source: https://x.com/cinbags/status/1546853506954711040
Your cures don’t work, therefore it’s the fault of the disease for not conforming:
Even though the past few decades have seen tremendous advances in our ability to treat the inflammation in autoimmune disorders with newer DMARDs and biologics, our patients overall are not faring much better in that the majority still have residual pain, fatigue, sleep and cognitive problems from the co-morbid FM that is present in many [51].
But over the past 50 years, there have been tremendous advances in our understanding of FM, and now it is widely studied by many groups of investigators and pain researchers worldwide. In fact, several years ago the most prestigious pain research organization worldwide, the International Association for the Study of Pain (IASP), formally voted to acknowledge that enough evidence had accumulated that FM is a very real disease, and coined the term nociplastic pain to describe the pain mechanism that is best exemplified by FM.
Pain = CNS, therefore it must be caused by the CNS!
The current understanding of nociplastic pain is that the central nervous system is the driving force behind this pain mechanism, and the key phenotypic features include widespread pain, fatigue, and sleep, memory, and mood disturbances [50,52].
These are also features of some autoimmune disorders, sometimes linked to Mg deficiency: the amplification of a stimulus and the steady progression of the disease:
On both quantitative sensory testing and functional neuroimaging there is evidence of amplification of painful stimuli as well as non-painful sensory stimuli (e.g. bright lights, odors, noises), and fairly consistently identified changes in functional connectivity that can even be noted in adolescents who are pain-free but go on to develop new widespread pain the following year [53].
Right, so you acknowledge that there is sub-clinical pathology, but you still won’t budge, because…
There is now acknowledgement that there is sub-clinical inflammation that is identifiable under ex-vivo provocation in nociplastic pain states, but it is much different in intensity and characteristics than the inflammation seen in autoimmune diseases.
Again, our “one-size-fits-all” allopathic tools don’t work, therefore it can’t be an autoimmune disorder:
And most importantly, this type of inflammation is apparently not successfully treated by the most powerful anti-inflammatories and immunosuppressive we commonly give our patients with autoimmune diseases and co-morbid FM [54].
You don’t see tissue inflammation or damage, therefore it has “none of the classic signs of an autoimmune disease”? Crude. Simplistic.
And perhaps most importantly, in FM classic inflammatory indices are normal (one suspects something other than FM when they are not), there is no objective evidence of inflammation on examination (e.g., synovitis), there is no identifiable tissue damage, and no evidence of tissue inflammation or damage. FM has none of the classic signs of an autoimmune diseases [1].
This isn’t disputed, and also doesn’t exclude immune dysfunction:
In contrast, FM is very similar to a large number of highly prevalent Chronic Overlapping Pain Conditions (COPCs). In addition to FM these include headaches, irritable bowel syndrome, temporomandibular disorder, low back pain, and many other common pain conditions [51].
There is a strong familial predisposition to developing these conditions, and individuals who have one of these conditions often meet criteria for many. These same conditions referred to as COPCs are generally those pain conditions considered by the most recent ICD criteria as “primary pain”.
WTF do they mean by “primary pain”? Is this just another name for an FND non-diagnosis?
This new designation means that the pain is considered the primary problem rather than being due to some other disease, e.g., a real autoimmune disease [55].
They used to think that bad smells caused disease too. There is certainly a bad bovine-excrement smell about a hypothesis that fails a Koch’s postulate-style disease transfer experiment.
The studies were “… not likely to be helpful” to your hypothesis!
There are several recent rodent studies that have purported to show that sera from individuals with FM can cause hyperalgesia or dorsal horn changes in rodents, but these studies are not likely to be helpful in determining whether FM is an autoimmune disease [32].
Very few acknowledged autoimmune disorders can be reproduced in animals simply by giving rodents sera or plasma from humans with that disease, and there are no valid animal models of FM [56].
“Overwhelming”? Seriously? You have already contradicted yourself in just a few paragraphs and needed to invent new causes such as “primary pain”.
Primary pain is also a non-diagnosis:
“Chronic primary pain is pain with no clear underlying cause, or pain (or its impact) that is out of proportion to any observable injury or disease.”15
You don’t what it is, but you sure know what it isn’t:
In light of this it is difficult to see how animal studies are going to counter the overwhelming clinical/human evidence that FM is not an autoimmune disease.
Then the arguments against become what can only be described as “childish”.
This rant confirms that the author still confuses inflammation and pain with autoimmunity.
This isn’t helpful, and it doesn’t explain away the observed phenomena in mouse studies and other research findings. PubMed alone returns 439 reports:
But for the sake of a vibrant debate, let us imagine for a moment that FM is an autoimmune disease. Then so is headache, irritable bowel, TMD, and low back pain – because it is widely acknowledged that the pathophysiology of these pain syndromes is similar. And coronary artery disease, psychiatric disorders, Type II diabetes, and most common medical problems are increasing acknowledged to have a mildly inflammatory component, but these are not considered autoimmune diseases. Aren't we bastardizing the term “autoimmune” if we use it carelessly or flippantly to describe anyone with any inflammation anywhere?
Vaccinal molecular mimicry goes hand-in-hand with increased risk of CVD.
Just saying, ahem:
Background: Some autoimmune diseases carry elevated risk for atherosclerotic cardiovascular disease (ASCVD), yet the underlying mechanism and the influence of traditional risk factors remain unclear.
Objectives: This study sought to determine whether autoimmune diseases independently correlate with coronary atherosclerosis and ASCVD risk and whether traditional cardiovascular risk factors modulate the risk.
… Conclusions: Autoimmune diseases were independently associated with higher burden of coronary atherosclerosis and higher risk for future ASCVD events, with risk accentuated by traditional cardiovascular risk factors. These findings suggest that autoimmune diseases increase risk through accelerated atherogenesis and that cardiovascular risk factor control is key for improving prognosis in patients with autoimmune diseases.
From: “Association of Autoimmune Diseases With Coronary Atherosclerosis Severity and Ischemic Events“ (2024)
Also:
Autoimmune diseases are associated with a dramatically increased risk of atherosclerotic cardiovascular disease and its clinical manifestations. The increased risk is consistent with the notion that atherogenesis is modulated by both protective and disease-promoting immune mechanisms. Notably, traditional cardiovascular risk factors such as dyslipidaemia and hypertension alone do not explain the increased risk of cardiovascular disease associated with autoimmune diseases.
From: “Autoimmune diseases and atherosclerotic cardiovascular disease“ (2024)
Moving swiftly on…
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Although not as prevalent as FMS, ME also affects more than a quarter million people in the UK.
Let’s see what our friends at the NHS have to say about it.
There are so many taboo subjects here that this guidance has not just one, but a herd of flippin’ elephants in the room.
You won’t see a word about vaccine A/Es, autoimmunity, gut dysbiosis, dietary deficiencies, or use of alternative therapeutics (such as from TCM):
Myalgic encephalomyelitis, also called chronic fatigue syndrome or ME/CFS, is a long-term condition that can affect different parts of the body. The most common symptom is extreme tiredness. The cause of ME/CFS is unknown.
ME/CFS can affect anyone, including children.
Symptoms of ME/CFS
The 4 main symptoms of ME/CFS are:
feeling extremely tired all the time (fatigue), which can make daily activities like taking a shower, or going to work or school, difficult
sleep problems, including insomnia, sleeping too much, feeling like you have not slept properly and feeling exhausted or stiff when you wake up
problems with thinking, concentration and memory (brain fog)
symptoms getting worse after physical or mental activity, and possibly taking weeks to get better (also called post-exertional malaise, or PEM)
Some people with ME/CFS may also have pain in different parts of the body or flu-like symptoms, such as high temperature, headache and aching joints or muscles.
The symptoms of ME/CFS are similar to the symptoms of some other illnesses, so it’s important to see a GP to get a correct diagnosis.
Find out more about the symptoms of ME/CFS
Diagnosing ME/CFS
There's no specific test for ME/CFS, so it's diagnosed based on your symptoms and by ruling out other conditions that could be causing your symptoms.
The GP will ask about your symptoms and medical history. You may also have blood and urine tests.
As the symptoms of ME/CFS are similar to those of many common illnesses that usually get better on their own, a diagnosis of ME/CFS may be considered if you do not get better as quickly as expected.
Find out more about diagnosing ME/CFS
Treating ME/CFS
While there's currently no cure for ME/CFS, there are treatments that may help you manage the condition and relieve the symptoms.
Treatments include:
energy management – where you're given advice about how to make best use of the energy you have without making your symptoms worse
medicine to control symptoms such as pain and sleeping problems
People with ME/CFS will need to adapt their daily routine and pattern of activities on a long-term basis. There may be periods when your symptoms get better or worse.
In other words: “go throw yourself off a bridge!” A real beacon of light. Thank you, NHS.
This load of tosh was last updated in May ‘24, and the next review isn’t until May ‘27. In the NHS, science progresses at a snail’s pace.
It’s so shockingly bad that they were even called out by a politician in 2022, albeit only because a relative was affected.
The wording implies that the NHS don’t believe it’s real. It’s great to see a request to investigate root causes. As with FMS, does the NHS think you are basically healthy underneath, and that they just need to manage your symptoms?
Health secretary pledges more ME/CFS research as he reveals that relative has condition
Rapid Response:
The missing piece in new treatment guidelines and research priorities for ME/CFS
In the UK, more than 250,000 people have Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) [1], a devastating illness that is estimated to cost the British economy £3.3 billion per year [2]. Although ME/CFS has long been maligned, three recent publications herald a dramatic change in the way it will be understood and treated in the UK.
As Ingrid Torjesen explains in her article 'Health secretary pledges more ME/CFS research as he reveals that relative has condition', the new NICE Guideline for ME/CFS [1] encourages a shift away from psychological and behavioural treatments. Consistent with this, research priorities published last month [3] call for a focus on biological mechanisms, diagnostic tests, and the development of medical treatments. Finally, the recent All-Party Parliamentary Group (APPG) report [4] outlines clear expectations of, and support for, a transformation in the way ME/CFS is addressed in research, clinical practice, and social care.
… While we applaud the new research priorities, it may be decades before biomedical breakthroughs are made or translated into effective, widely available treatments for ME/CFS [22]. Similarly, while the APPG report sets a clear expectation for improved health and social care provision for people with ME/CFS, that change is likely to be slow. In the meantime, families will continue to provide the majority of care for people with ME/CFS and bear the physical, psychological, and economic scars of doing so.
-In loving memory of Maeve Boothby O’Neill, 27, for whom change came too late-
It’s not a huge cash cow for Big Pharma, partly because they don’t know what drugs to use as a treatment, even for suppressing symptoms.
It’s also another “non-diagnosis” label for what medicine cannot explain:
Global Chronic Fatigue Syndrome Treatment Market Report 2023: Sector is Projected to Reach $68.2 Million by 2031 at a CAGR of 4.2%
The global chronic fatigue syndrome treatment market size was valued at USD 47.2 million in 2022 and is projected to grow at a CAGR of 4.2% during the forecast period of 2023-2031 to reach a value of USD 68.2 million by 2031.
Key Players in the Global Chronic Fatigue Syndrome Treatment Market
The report provides a detailed analysis of the key players involved in the chronic fatigue syndrome treatment market, including their business overview, product portfolio, recent developments, and financial analysis. Some of the major players operating in the market include:
Hemispherx Biopharma
GP Pharm
Cadila Pharmaceuticals
USV
Torrent Labs
Goodfellow Pharma
F. Hoffmann-La Roche Ltd
The market growth can be attributed to the increasing prevalence of chronic fatigue syndrome and the rising awareness about the condition.
Chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis (ME), is a complex disorder characterized by extreme fatigue that cannot be explained by any underlying medical condition. The fatigue is worsened by physical or mental activity and does not improve with rest.
Treatment options for CFS include medication, counselling, and lifestyle changes to manage symptoms and improve the quality of life for patients. The increasing prevalence of CFS, rising awareness about the condition, and the growing demand for effective treatment options are driving the market growth.
… The chronic fatigue syndrome treatment market is expected to continue to grow in the coming years, as awareness of the condition continues to increase, and new treatment options and technologies are developed to meet the needs of patients with CFS.
Epidemiology of Chronic Fatigue Syndrome
Chronic fatigue syndrome affects millions of people worldwide, with varying prevalence rates reported across different countries and regions. According to the Centers for Disease Control and Prevention (CDC), an estimated 836,000 to 2.5 million Americans suffer from CFS but majority of them remain undiagnosed. In Europe, the estimated prevalence of CFS ranges from 0.4% to 2.5% of the population. In Asia, the prevalence of CFS is reported to be lower, ranging from 0.2% to 1.2%.
It affects both genders, but it is more prevalent among women than men. Women are reported to be two to four times more likely to develop CFS than men. The condition can affect individuals of all ages, but it is most diagnosed in people between the ages of 40 and 60. Chronic fatigue syndrome can also affect children and adolescents, but it is less common in these age groups.
From: “Global Chronic Fatigue Syndrome Treatment Market Report 2023: Sector is Projected to Reach $68.2 Million by 2031 at a CAGR of 4.2%“ (2023)
A new perspective
I came across this paper whilst reviewing related literature for “Cancer Megathread #34: SARS-CoV-2, synthetic spike protein and heat shock protein mimicry”:
Ryabkova et al. published “Autoantibody Correlation Signatures in Fibromyalgia and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Association with Symptom Severity" on 18th January 2023 in the MDPI journal “biomedicines”16.
Synopsis
Recent studies into the contribution of autoantibodies (AAb) to autoimmune mechanisms of FMS and ME/CFS paid the most attention to pathogenic AAbs that target G protein-coupled receptors. But, to date, most studies have ignored the possible involvement of an extensive network of natural AAbs in these disorders.
What the study involved
Immunoassays were used to determine the serum levels of 33 natural AAbs to neural, organ-specific, and non-tissue-specific autoantigens of 33 study participants, grouped into 3 cohorts:
11 ME/CFS patients comorbid with FMS.
11 ME/CFS patients without FMS.
11 healthy controls.
Levels were indexed against a reference control sample derived from a pool of 5000 healthy individuals, and a range of values was determined for each of the 33 antigens to represent what was considered to be the normal range.
Once the AAb profiles were determined, these were then compared against scores for symptoms associated with these conditions to create correlation patterns, i.e. which AAbs patterns were associated with self-reported levels of fatigue, anxiety, bodily pain, depression, and physical and metal health-related quality of life when compared to the healthy controls.
If the null hypothesis was correct - that autoimmune antibodies are not involved mechanistically in these conditions - there should have been no correlational patterns.
The conclusions drawn from their analysis are profound, and it’s shocking to compare their findings with the NHS's approach and accepted guidance.
Because natural autoAbs were thought to be only associated with healthy individuals, it is easy to see why these have been overlooked until now: as potential causes of disease when present within a normal range.
Background and Definitions:
GPCRs: G protein-coupled receptors. Not all autoAbs are bad. In this example, aAbs help to prevent a systemic reaction to an acute local injury by blocking some of the chemo-attractant molecules called chemokines:
… AutoAbs against GPCRs activate these receptors that amplify the inflammatory responses through their signaling pathway.
Releasing mediators from smooth muscle cells and accumulating inflammatory cells cause severe vascular dysfunction (vasculopathy).
Further endothelial damage and fibroblast conversion to the myofibroblast and extracellular matrix (ECM) deposition initiate the fibrotic process (fibrosis), which causes vessel stenosis and obliteration.
… Abs against GPCRs such as AT1R, ETAR, CXCR3, and CXCR4 can attract immune cells that express the corresponding receptors or be attracted by those cells, which is similar to the interaction of endogenous ligands to their receptors (8, 13, 19, 20). These effects seem to be important in immune cell homeostasis between blood and tissues, in which a balance between the serum levels of Abs against GPCRs and GPCR expression of immune or tissue-resident cells regulate cell migration towards the tissues and therefore prevent a systemic immune response to an acute local injury (21).
From: “When natural antibodies become pathogenic: autoantibodies targeted against G protein-coupled receptors in the pathogenesis of systemic sclerosis“ (2023)
- Another name for fibromyalgia is “fibrosis syndrome”. AutoAbs against GPCRs are typically associated with systemic sclerosis (as above), primary Sjogren’s syndrome or systemic lupus erythematosus (SLE).
The paradox is that some autoimmune disorders involve lower than normal levels of some autoAbs. No wonder the professor lost his shi cool:
… In contrast, some diseases including autoimmune diseases are characterized by reduced levels of GPCR abs when compared to healthy donors. Thus, patients with giant cell arteritis have lower ETAR ab levels compared to healthy donors (24) and patients with granulomatosis with polyangiitis have reduced levels of antibodies against complement receptors (2).
Furthermore, reduced levels of antibodies against ß1-adrenergic receptors are present in patients with acute coronary syndrome and are associated with a more severe disease particularly with a higher risk for early reinfarction and cardiovascular death in patients ≤ 60 years (25, 26).
Lower abs against the thrombin receptor PAR-1 are associated with ovarian cancer and with high-grade carcinoma (2, 27).
Finally, decreased levels of abs against the chemokine receptor CXCR3 and CXCR4 are found in patients with progressive interstitial lung disease (28, 29).
The presence of both increased as well as reduced GPCR ab levels further strengthen the idea of the presence of physiological levels and a balanced generation of autoantibodies in human physiology and pathophysiology.
… Abnormally Reduced G Protein-Coupled Receptor Antibodies as Biomarkers for Acute Damage and Possible Drivers for Vascular Damage
In comparison to healthy donors, GPCR ab levels can also be reduced. As mentioned above, GPCR ab levels are in a tight balance with the general and chronic expression status of their corresponding GPCR, which can be up- or downregulated. Downregulation could result in a reduced GPCR ab response.
From: “What Makes Antibodies Against G Protein-Coupled Receptors so Special? A Novel Concept to Understand Chronic Diseases“ (2020)
https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.564526/full
HC: Healthy controls.
“Natural autoantibodies are normal components of the humoral arm of the immune system found in clinically healthy individuals.”17
- These include natural anti-viral/antibacterial IgG, mucosal IgA, and the first-line blood/lymph antibodies IgM.
On the other hand, some so called “pathogenic” aAbs may also form part of our anti-cancer adaptive immunity:
Pathogenic aAbs are defined as immunoglobulins contributing to the development of an autoimmune disease and its organ and/or systemic manifestations. If the lack of pathogenicity is demonstrated for an aAb, it is referred to as non-pathogenic.
Pathogenetic aAbs are immunoglobulins present during the development of an autoimmune disease and its organ and/or systemic manifestations but not known, or demonstrated to, contribute to the pathophysiological process.
For example, anti-RNAPIII aAbs may originate as an anti-cancer immune response to mutated cancer epitopes, thus providing an important clue to the origin of these immunoglobulins. 53 Yet, no experimental evidence suggests that anti-RNAPIII are pathogenic per se and therefore, in the current state of knowledge, they are best classified as pathogenetic aAbs.
… Natural aAbs
Natural aAbs are immunoglobulins that are present in serum from healthy individuals and that react with self-molecules, including DNA, nuclear and cytoskeletal proteins, and cell-surface aAgs (Table 1).
Although emphasis has been on IgM natural aAbs, isotypes of natural aAbs encompass immunoglobulin G (IgG) and immunoglobulin A (IgA) as well.57–59
In fact, natural IgG and IgA are predominant serum and mucosal natural aAbs.57–60 They are encoded by unmutated V(D)J genes and display weak to moderate affinity for self-antigens.
Natural antibodies, notably of IgM isotype, which represent a considerable amount of the total IgM circulating in humans, provide a first line of defense against infections, serve housekeeping functions, contribute to the homeostasis of the immune system,5,61,62 and act as protective aAbs notably by being anti-apoptotic.63–65
… To evaluate whether an aAb in SSc is truly pathogenic, scientific criteria for pathogenicity are needed. In 1993, Naparstek and Plotz 1 proposed such criteria on the premise that: “To establish that an autoantibody is pathogenic, one must be able to construct a plausible picture of how it might act and to reproduce it experimentally.”
From: “Pathogenic roles of autoantibodies in systemic sclerosis: Current understandings in pathogenesis“ (2019)
As you can see, it is far too simplistic to equate autoimmune disease just to the presence of inflammation and high levels of pathogenic autoAbs.
Ryabkova et al. take discussions to the next level and expand on this.
A walkthrough of “Autoantibody Correlation Signatures in Fibromyalgia and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Association with Symptom Severity":
Abstract
Recent studies provide some evidence for the contribution of antibody-mediated autoimmune mechanisms to the nature of fibromyalgia (FM) and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Much attention was paid to the autoantibodies (AAb) targeting G protein-coupled receptors as natural components of the immune system. However, the natural AAb network is much more extensive, and has not been previously investigated in these disorders.
The enzyme immunoassays ELI-Viscero-Test and ELI-Neuro-Test were used to determine changes in serum content of 33 natural AAb to neural, organ-specific and non-tissue-specific autoantigens (a) in 11 ME/CFS patients with comorbid FM; (b) in 11 ME/CFS patients without FM; (c) in 11 healthy controls. Individual AAb profiles and their correlation with some clinical symptoms were analyzed.
The first finding is that, despite the low n-number of participants, they found a link between ME/CFS and autoAbs, despite the accepted cause being “unknown”:
Both patients with ME/CFS(−)FM and ME/CFS(+)FM were characterized by more frequent and pronounced deviations in the immunoreactivity to GABA-receptors than healthy controls.
Both groups had altered AAB correlation signatures when compared to the HCs:
Although the level of other natural AAb did not differ between study groups, AAb correlation signatures were altered in patients compared to healthy controls.
Despite being “healthy”, “natural” AAbs, different correlation patterns correlated with different disease symptoms.
If you are only test for pathogenic aAbs then you might not find anything unusual.
Both in patients and healthy controls the level of natural AAb to various neural and tissue-specific antigens correlated with the severity of fatigue, bodily pain, depression, anxiety, physical and mental health-related quality of life.
Notably, widely different correlation patterns were observed between study groups.
Findings from this pilot study provide some evidence that the homeostasis of autoimmune relationships, which are possibly a physiological part of our immune system, may be altered in FM and ME/CFS.
The correlation of disease-induced perturbations in individual AAb profiles with some clinical symptoms may arise from the immune system’s ability to reflect qualitative and quantitative changes in antigenic composition of the body.
1. Introduction
Fibromyalgia (FM) is a common cause of chronic, widespread, musculoskeletal pain with unclear etiopathogenesis. However, it was demonstrated in a recent breakthrough study that IgG from the patients with FM produced painful sensory hypersensitivities by sensitizing peripheral nociceptive afferents in mice [1].
FM and ME/CFS have overlapping symptoms, and often that extends to the diagnosis too. This strongly leads you to a hypothesis of there being common root causes:
The common core symptoms of fatigue, sleep problems, and cognitive difficulties lead to significant comorbidity between FM and ME/CFS, but it can vary depending on the diagnostic criteria used [4].
While in one study 34% of 313 patients diagnosed with ME/CFS had comorbid FM according to the American College of Rheumatology (ACR) old diagnostic criteria of 1990, the other research group reported that the prevalence of FM among patients with ME/CFS could reach 50% when ACR 2010 newer diagnostic criteria were applied [4].
The recent meta-analysis confirmed a prominent clinical overlap between FM and ME/CFS [5].
Mitochondrial impairment is one explanation for symptoms of fatigue. This suggests considering melatonin, baicalein or methylene blue for a therapeutic shortlist.
Although the exact pathogenesis of ME/CFS is still unknown, according to the most widely held hypothesis, it is a complex multifactorial syndrome with immunological, metabolic, mitochondrial, autonomic and adrenal dysfunction as the key pathogenetic mechanisms [6,7].
Calling the NHS specialists and media content creators:
Emerging evidence suggests that disorders of autoimmunity play an important role in postinfectious ME/CFS, and that targeting AAb could be a promising treatment approach [8,9].
The tail can wag the dog too. I.e. autoantibody levels may reflect corresponding antigen levels:
At the same time, an increased level of any AAb in the serum of a patient is not an ultimate sign of autoimmune disease, but can indicate changes in expression and/or excretion of the corresponding antigens [8]. From this point of view, not only increased, but also decreased levels of AAb are relevant.
They defined normalised levels of organ-specific and non-specific AAbs:
2. Materials and Methods
We defined individual normalized levels of AAb against 21 organ-specific and non-organ-specific antigens and 12 neural antigens using standardized ELISA test systems for semi-quantitative serum AAb evaluation (ELI-Viscero-test-24 and ELI-N-test-12 by Medical Research Center “Immunculus”, Moscow, Russia). The antigens used in the test systems are listed in Table 1.
Table 1 lists the 33 antigens:
Immunoglobulins in the control serum were obtained from the blood serum of more than 5000 healthy donors, and brought to a concentration close to physiological (16 mg/mL). Thus, pooled control serum contained population-normalized IgG class polyclonal antibodies to each of the studied antigens, and was used as a universal standard for all tested antigens.
AAb to antigen levels were thus referenced to this pooled control serum:
Depending on the studied antigen, the pooled control serum was diluted to a final concentration, which was derived on the basis of studies of the level of AAb of a large cohort of individual serum samples from healthy donors. The content of AAb to the studied antigens was evaluated in the conventional units of optical density, and compared to their content in a control pool of sera from healthy donors (taken for 100%).
The body mass index (BMI) of patients with both ME/CFS and FMS was lower than the other groups:
Patients from ME/CFS(+)FM and ME/CFS(−)FM groups did not differ from controls in terms of gender and age. While BMI in ME/CFS(−)FM group was similar to the BMI in HC, it was significantly lower in ME/CFS(+)FM group. Regarding race and ethnicity, all patients and HC were Caucasian and not Hispanic.
Most of the patients have been suffering for years:
The illness duration varied, with a range of 1 to 35 years and median value of 6.0 years in the ME/CFS(+)FM group and with a range of 2.5 to 35 years and median value of 7.0 years in the ME/CFS(+)FM group.
A third of the ME/CFS patients with FMS, and 73% without, reported infection-triggered onset:
Four patients (33%) with ME/CFS and comorbid FM and eight patients (73%) without comorbid FM reported an infection-triggered onset of disease.
All the patients had post-exertional malaise:
It should be noticed that all patients in our study presented with clinically significant post-exertional malaise (according to the DSQ-SF, they had frequency and severity ratings ≥2 in questions number 2 or 3), which has been considered a key symptom of ME/CFS for over three decades [10,11,12].
Depression and anxiety were common to both groups:
Depression and anxiety levels were significantly higher in ME/CFS(−)FM and ME/CFS(+)FM groups. The median HADS-D subclase score indicated probable comorbid depression only in the ME/CFS(+)FM group, and the median HADS-A score corresponded to borderline anxiety in both groups of patients.
AAb correlations were mapped:
(a) ME/CFS(−)FM (n = 11)
(b) ME/CFS(+)FM (n = 11)
(c) healthy controls (n = 11)
To identify changes in the AAb relationships in patients suffering from ME/CFS with and without concomitant FM, we analyzed AAb correlations in the two patient groups separately. A number of correlations between the absolute R(dev)agNs values in both groups were revealed. Disease-specific changes among the studied AAb were identified (Figure 1a,b).
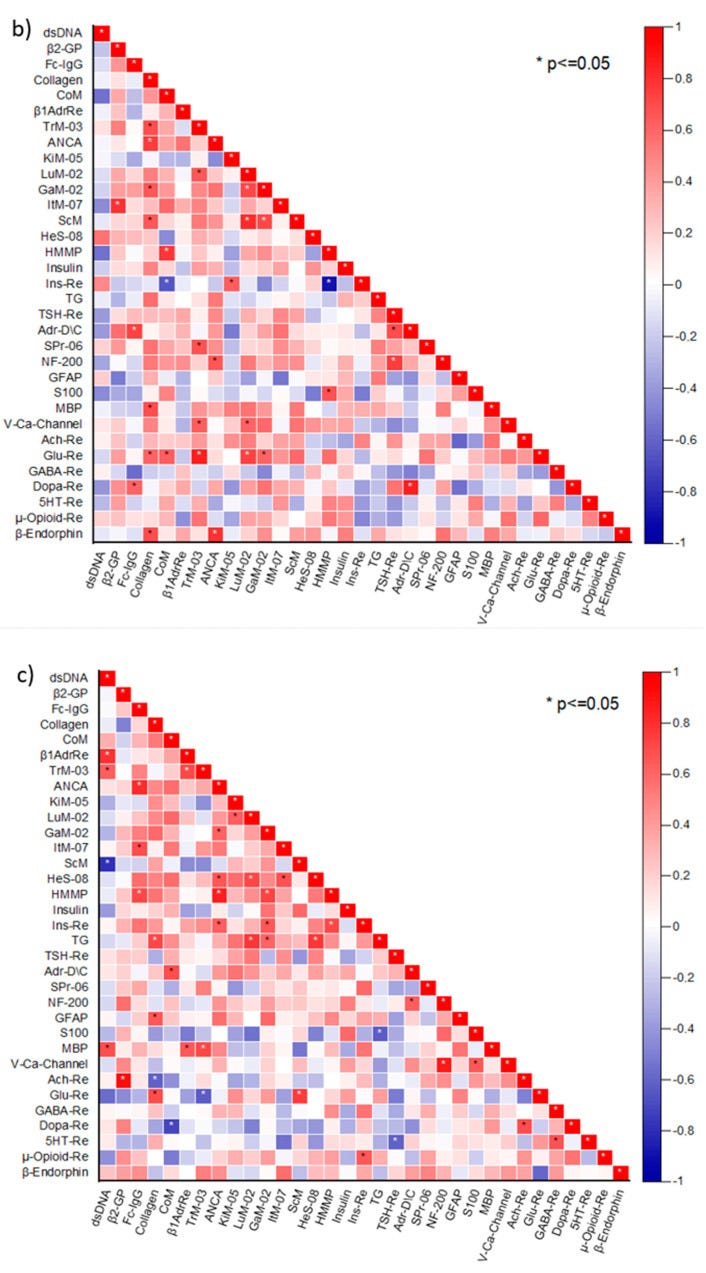
These heatmaps demonstrate that levels of natural AAbs correlate with disease:
The aforementioned data on the correlation between R(dev)agNs and some symptom scores, even in HC, suggested the presence of physiological relationships among natural AAb.
4. Discussion
It has been suggested that autonomic nervous system imbalance might be causing the symptoms in these conditions and, in turn, might be triggered by the pathogenic functional AAb [21].
At the same time, it should be kept in mind that the presence of AAb does not imply the presence of an autoimmune condition, as AAb are also recognized in non-autoimmune diseases [22,23].
Just because they may attack “self” doesn’t make them pathogenic:
According to the modern interpretation of the phenomenon of physiological autoimmunity, AAb act as adaptive bioregulators of cell functions and growth along with neurotransmitters and hormones, both in health and disease [24].
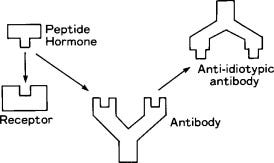
Not only do we need a balance of both natural and pathogenic AAbs, but we also have a network of antiidiotypic antibodies that can bind them. Good luck obtaining and analysing meaningful lab results from all this.
“An antiidiotypic antibody is defined as an antibody that possesses an epitope in common with a foreign antigen, allowing it to mimic biological properties of specific receptors and be used for immunotherapy against certain tumors.”18
“The immunculus is considered as the system (general network) of constitutively expressed natural autoantibodies against different extracellular, membrane, cytoplasmic, and nuclear self-antigens (ubiquitous and organ-specific). It is specially noted that the repertoires of natural autoantibodies are surprisingly constant in healthy persons, independent of gender and age, and characterized by only minimal individual peculiarities (individual immune fingerprints). On the other hand, abnormal metabolic changes which precede the clinical manifestation of different diseases showed easily detected changes, rather quantitative than qualitative, in the systems of natural autoantibodies in patients' sera (immunculus distortions).”19
Moreover, there is a concept of “Immunculus” or “Immune Homuculus” based on the assumption that the network of physiological autoreactive antiidiotypic AAb may dynamically reflect the whole individual antigenome as a totality of internal immunological images of the autoantigens [25,26,27].
It’s not about autoimmunity, but “dysregulated natural autoimmunity”. From this perspective, the current NHS allopathic approach to diagnosis and treatment needs a complete review:
The results obtained in our study suggest that ME/CFS and FM are rather not autoimmune diseases, but conditions with dysregulated natural autoimmunity.
AutoAbs to GABA Re were not significantly different to those of the HCs:
In particular, while 54.5% and 45.5% of patients in ME/CFS(+)FM and ME/CFS(−)FM groups presented with abnormal absolute deviations of serum reactivity against GABA Re compared to none in the control group, these changes were not very pronounced (since no significant differences have been observed in median R(dev)agNs between the three groups).
Although elevated levels of pathogenic AAbs were initially associated with disease, these levels tended to normalise after the first 3 years (i.e. lab tests coming back normal).
Despite this, over 90% of patients never fully recover:
Classical autoimmune diseases with pathogenic AAb are characterized with a significant increase in the level of the AAb. While immunological and inflammatory changes have been repeatedly reported in many ME/CFS patients, these changes tend to be most pronounced during the first 3 years of the disease [28].
However, according to the longitudinal studies of varying duration, less than 10% of patients with ME/CFS fully recover [3]. These findings support the hypothesis that not pathogenic AAb, but dysregulated natural autoimmunity is of crucial importance in the pathogenesis of ME/CFS.
According to the concept of physiological autoimmunity, quantitative changes in the content of natural AAb are related to variations of expression and secretion of the relative antigen, reflecting functional state of the corresponding cell type [19,27].
“Glutamate is the major excitatory neurotransmitter in the nervous system. Glutamate pathways are linked to many other neurotransmitter pathways, and glutamate receptors are found throughout the brain and spinal cord in neurons and glia. As an amino acid and neurotransmitter, glutamate has a large array of normal physiological functions. Consequently, glutamate dysfunction has profound effects both in disease and injury.”20
GABA antagonises the effects of glutamate:
“Gamma-aminobutyric acid (GABA) is an amino acid that functions as the primary inhibitory neurotransmitter for the central nervous system (CNS). It functions to reduce neuronal excitability by inhibiting nerve transmission. GABAergic neurons are located when the hippocampus, thalamus, basal ganglia, hypothalamus, and brainstem. The balance between inhibitory neuronal transmission via GABA and excitatory neuronal transmission via glutamate is essential for proper cell membrane stability and neurologic function.”21
GABA Re is an element of endogenous stress-regulating mechanisms preventing distress [29]. The last factor has long been considered as increasing the risk of ME/CFS [30]. An imbalance between excitatory and inhibitory neurotransmission has been linked to ME/CFS and FM [31].
The authors helpfully suggest some potential therapeutics to rebalance glutamate : GABA neurotransmission:
Regarding some potential substances for future clinical research in ME/CFS and FM, it should be mentioned that a number of complementary dietary supplements have been reported to rebalance glutamate:GABA neurotransmission, namely Omega-3 PUFAs, CoQ10, Withania Somnifera (Ashwagandha, Indian Ginseng), N-acetylcysteine, vitamin B12, curcumin (contained in turmeric), zinc, magnesium, 2-aminoethanesulfonic acid (L-Taurine), and carnitine (L-Carnitine) [32].
The authors found that the main target of the aAbs was the nervous system, as expected:
The majority of AAb, for which significant correlations with the symptom scores were identified in HC, target neural antigens, which was expected as the analyzed symptoms are neuropsychological.
Both ME/CFS cohorts also had aAbs which targeted internal organs, or were non-specific:
This association was disturbed in both ME/CFS(+)FM and ME/CFS(−)FM groups—the number of AAb targeting internal organ-specific and non-tissue specific antigens correlated with the symptoms scores in these groups.
It’s not all in your head, and autoimmune dysfunction has been demonstrated for both ME/CFS and FMS:
Thus, our findings allow us to assume that ME/CFS and FM are organic multisystem diseases, rather than psychological disorders.
Look after your gut microbiome, liver, kidneys, and diet:
The pattern of correlations found in ME/CFS(−)FM (according to the manufacturer of the ELI-tests) suggests the roles of the gut microbiome, disturbed detoxification mechanisms (namely, liver and kidney functioning), and an inflammatory process in the pelvic organs in the development of symptoms.
The mechanisms remain unclear, but neurotransmitter dysregulation is clearly implicated:
… the mechanisms underlying the observed correlations remain largely unclear and can differ between patients and HC. For example, anti-GABA-Re AAb were associated with a lower mental component score, i.e., worse self-perceived mental health in HC, while in patients from the ME/CFS(−)FM group, these AAb were inversely correlated with depression.
In other words, normal levels of β-endorphin lead to an autoimmune response which disrupts your natural pain-supressing opiates:
Changes in immunoreactivity to β-endorphin were associated with more pronounced fatigue in both ME/CFS(−)FM and ME/CFS(+)FM groups, but not in HC. These findings suggest the dysfunction of the endogenous opioid system in ME/CFS and FM.
Why CBD and THC are beneficial22:
Interestingly, a significant factor that differentiates β-endorphin from other endogenous opiates is its high affinity for and lasting effect on μ-opioid receptors [33].
It was shown by Schrepf et al., in the study employing PET and fMRI together, that dysregulation of the endogenous opiate system in FM could lead to less excitation in antinociceptive brain regions by incoming noxious stimulation [34].
Hyperalgesia: Increased sensitivity to pain, and previously non-painful stimuli.
Allodynia: Similar to hyperalgesia, a type of neuropathic pain which may result from previously non-painful stimuli or a light touch or contact on the skin.
Hyperalgesia and allodynia commonly observed in this population were consistent with the imaging findings.
GFAP: Glial fibrillary acidic protein.
“GFAP is a key intermediate filament (IF) III protein responsible for the cytoskeleton structure of glia cells and for maintaining their mechanical strength, as well as supporting neighboring neurons and the blood brain barrier (BBB)”23.
You can imagine why AAbs to this would contribute to a plethora of mental health-related symptoms in FMS and ME/CFS patients:
Increasing evidence suggests that GFAP might be a biomarker for a number of neurological conditions, which is characterized by strong brain-specificity and high expression level in the brain.
Brain injury causes the release of GFAP and its breakdown products from injured astrocytes to the extracellular space, where these proteins equilibrate into the subarachnoid CSF compartment, then release into the circulating blood by the glymphatic pathway or by diffusing past the (possibly compromised) brain blood barrier [35].
It has been also reported that GFAP can serve as an autoantigen, triggering AAb response in a subset of patients [35].
In our study, changes in anti-GFAP AAb level were positively associated with worse mental component score in the ME/CFS(+)FM group and with illness duration in the ME/CFS(−)FM group.
Regarding mobility, they also found a correlation between anti-collagen AAbs and hypermobility syndrome (joints with a greater than normal range of movement, which can contribute to mobility issues and pain):
The ME/CFS(+)FM group was characterized by an increase in the number of associations of anti-collagen AAb and anti-TrM-03 AAb with other AAb.
It has been recently reported that 81% of patients with ME/CFS and/or FM met Brighton criteria for hypermobility syndrome, and 18% met 2017 hypermobile Ehlers–Danlos syndrome criteria.
The authors then discussed the major limitations of the study. These included a small sample size, the absence of a single case definition of ME/CFS, and they didn’t exclude the presence of other comorbidities that are frequently associated with both conditions. For example, irritable bowel syndrome (IBS) or postural orthostatic tachycardia syndrome (POTS) may also affect natural AAb patterns.
No conflicts of interest were declared.
More: https://pmc.ncbi.nlm.nih.gov/articles/PMC9952981/
Parting shots
NewsGuard. Again.
USAID Censorship Scheme Exposed; Global Engagement Center Worked With UK Government And Media Firms To Deploy AI Tools
On Thursday, America First Legal (AFL) released explosive new documents obtained through ongoing litigation against the U.S. Department of State’s Global Engagement Center (GEC), exposing a vast, government-backed censorship operation to silence Americans under the guise of “misinformation,” “disinformation,” and “malinformation.” The documents reveal a disturbing alliance between the GEC, the U.S. Agency for International Development (USAID), the British Foreign, Commonwealth, Development Office (FCDO), and media censorship organizations, all working in lock-step to manipulate public discourse, control media narratives, and suppress free speech.
… II. Coordination with Internet Censors NewsGuard and Poynter
Two days after the 2020 U.S. Presidential election, NewsGuard Technologies’ General Manager, Matt Skibinski, started an email chain to pitch NewsGuard services. Included in this email chain were:
Park Advisors’ then-Director Christina Nemr is an Obama Administration State Department alum. According to her LinkedIn, Park Advisors “Designed and led multi-million public-private initiatives addressing security threats in the information environment, bridging gaps between emerging technologies and real-world operational needs. Built and managed a global platform that evaluated and connected tools with mission-critical challenges, supporting government adoption.”
The House Small Business Committee found that Park Advisors received a GEC cooperative agreement award of more than $6 million. Park Advisors then distributed subawards to several companies, including NewsGuard, the Atlantic Council, and the Global Disinformation Index, a project funded by George Soros that generated lists of conservative websites it urged advertising companies to boycott. Together, these groups, not subject to international restrictions like GEC was, tested disinformation products, which led to the creation of the “Disinfo Cloud,” an unclassified platform used by the U.S. federal government, the European Union, the U.K. government, the Australian government, and the Estonian government “to counter adversarial propaganda and disinformation.”
Government employees from the Department of State, the National Security Agency (NSA), and Department of Defense components, including the National Security Innovation Network (NSIN), U.S. Cyber Command, and the U.S. Army European Command.
… While NewsGuard claims to be a fair arbiter of truthfulness, research by the Foundation For Freedom Online reveals how NewsGuard operates the enforcement arm of the censorship industry that rates websites based on how much “misinformation” each site publishes.
The Thought Police haven’t gone away.
We live under increasingly totalitarian regimes, with freedom of speech under greater threat than ever.
My new X account was nuked within minutes of posting a link to the latest saRNA Substack. I didn’t even post the title or description, just a screenshot.
They wouldn’t cite the “offence”, and my appeal went unanswered, but I suspect it was linked to the UK’s Online Safety Censorship Bill, and the dystopian EU vultures sensing blood:
EU Could Fine Musk's X $1 Billion Over Illicit Content, Disinformation
European Union regulators are reportedly mulling a $1 billion fine against Elon Musk’s X, taking into account revenue from his other ventures, including Tesla and SpaceX, according to The New York Times.
Even Substack isn’t immune. They can defund you by targeting the payments system “Stripe.” All it takes is one call from the Brownshirts.
Parents Arrested In UK For Complaining About Their Kid's School In WhatsApp Group
The parents of a nine year old British girl were arrested by police who came to their home after they complained about their child’s school in a WhatsApp chat group.
Yes, really.
The Times reports that Police arrested Maxie Allen and Rosalind Levin in front of their daughter on suspicion of malicious communications, harassment, and causing a nuisance on school property.
The pair were thrown in a jail cell over comments they made about the Cowley Hill Primary School in Borehamwood,
The report notes that the parents had taken issue with the school’s process of hiring a new head teacher, with school governors stepping in and issuing them with a warning for causing “disharmony”.
The school later completely banned the parents from the premises and were told they could only communicate via email.
The parents were then allegedly accused by the school of making “disparaging” remarks about the institution and “casting aspersions” in a parents’ group on WhatsApp, prompting the school to contact police.
The police then ordered the parents to remove their child’s from the school, which they did, yet they were still arrested a week later on their own doorstep and kept in jail for 11 hours.
Citing BS Study, WebMD Claims COVID Vaxx ‘Still Crucial’ For Kids
… Francis Collins ‘fears for the future of science’
He’s also still pimping the line that COVID-19 emerged from a natural penguin-on-bat interspecies gang rape or whatever.
Related: Ousted Director Francis Collins Demands Americans Pay ‘Utmost Respect’ to NIH
… Via TIME (emphasis added):
“I've been increasingly concerned about the polarization of our society, and that goes back even before COVID. But COVID brought it out in a particularly troubling way, where information that might have been lifesaving, such as the use of the vaccines, did not always land with people who had already been influenced by lots of other misinformation*, or even disinformation, coming from social media, cable news, and sometimes politicians. So when I stepped down as NIH director, I began the effort to try to put together a book called The Road to Wisdom. It focuses particularly on the topic of truth: that there really is such a thing as objective truth. A society that decides truth is just how you feel about it, and that alternative facts are okay, is heading into a very dangerous place. And it feels like that's sort of where we are.”
“Influenced by misinformation,” you say?
I somehow don’t recall Francis Collins bringing that same energy when his own colleagues lied, repeatedly, for years, with no pushback from the government at large or the mainstream so-called news media, about the origins of the pandemic, the efficacy of the shots they called “vaccines,” or the rules they invented out of thin air like “six feet to stop the spread.”
… WebMD COVID vaccines
Via Web MD (emphasis added):
“Vaccinated children are much less likely to develop “long COVID” than are unvaccinated children, according to a new study that researchers hope will convince parents to keep kids’ immunizations up to date.
Many parents don’t get their children vaccinated against COVID-19 because pediatric cases are generally mild. But the study of post-COVID condition (PCC), as scientists call long COVID, supports continued vigilance*, researchers say.”
*”Continued vigilance” being a euphemism for “continued terror.”
Related: Leaked: Trump CDC to Probe Long-Rumored Vaccine-Autism Link
Continuing:
“The new study looked at children ages 5 to 17 in four states from July 2021 through May 2023. If they’d been vaccinated prior to infection, their chances of developing one or more PCC symptoms were reduced by 57%...
Of the 622 children who had at least one positive COVID test during the study period, 28 (5%) reported PCC symptoms and 594 (95%) didn’t report any during the follow-up period.”
This is how you know it’s bullshit: of all the previously healthy children you know and see around, how many do you know of in your personal life who have experienced “long COVID”? Is it anywhere approaching 5%?
Lived experience always trumps rigged studies sponsored by the Public Health™ establishment.
Then the punchline: “Of the children with PCC in the study, 57% had been vaccinated.”
I had to read that line, and reference the actual study, to make sure I understood correctly that, in a study allegedly finding that COVID vaxxes are “crucial” for kids so they don’t get Long COVID, 57% of the kids with Long COVID were actually vaxxed.
That’s called The Science™, boys and girls, and it’s beyond reproach.
WebMD (funded by the pharmaceutical industry) wouldn’t lie to you.
WebMD loves you and your children.
WebMD wants you to live a long, healthy, happy life.
Vaccine Stocks Tank, Moderna Craters After FDA Biologics Head Abruptly Steps Down
Vaccine stocks tumbled in the early U.S. cash session after Peter Marks—a top FDA regulator and pro-vaxxer—abruptly resigned on Friday.
… Moderna shares are also down 95% from peak Covid highs.
Further reading:
Health insurance CEO admits to hiring private investigators to dig up dirt on patients, doctors and politicians
The CEO of a Texas health insurance company was fired after admitting before a DOGE panel of state lawmakers that he hired private investigators to spy on customers and obtain sensitive details about their lives.
… “The allegations concerning Superior’s actions, such as actions that were characterized as potentially blackmailing lawmakers to secure state contracts and surveilling private citizens to avoid paying legitimate claims, are deeply troubling,” he said in a statement.
Vivid nightmares precede lupus diagnosis by over a year in some patients
… Nightmares could potentially signal the start of a flare for some patients with the autoimmune disease lupus, new research hints.
For some patients, this uptick in vivid bad dreams began over a year before they experienced any symptoms commonly tied to lupus, such as joint pain and rashes. Their "horrific" nightmares often involved falling or being attacked, trapped or crushed, they said.
These new findings do have some limitations, as they're drawn solely from surveys and interviews — but they may begin to unravel experiences commonly reported by people with lupus.
"Neuropsychiatric symptoms are often talked about between patients in online support groups," said lead author Melanie Sloan, a researcher in the Department of Public Health and Primary Care at the University of Cambridge. "But we previously found that they were rarely or never reported to their doctors by over half of patients."
In the study, published May 20 in the journal eClinicalMedicine, Sloan and colleagues probed neurological and psychiatric symptoms — such as depression, anxiety, cognitive dysfunction and disturbed dreaming — in people with systemic lupus erythematosus. This disease is characterized by inflammation and damage to bodily tissues.
IgG4 class switching, vaccine flops, and the rest:
Winter virus levels remain higher than usual despite warm weather
The number of people in hospital in England with winter viruses remains higher than usual for the time of year, despite the recent warm and sunny weather, new data shows.
Norovirus and flu levels have yet to drop as low as is typical for this point in spring and the amount of Covid-19 patients being treated on wards is at its highest so far in 2025.
The figures come as England’s chief medical director admitted “far too many” people waited too long for hospital care this winter, while Health Secretary Wes Streeting said the Government was “already working” to learn lessons from the past few months.
It should have been called “Strictly Come Vaccinated”.
Tom joins a long list of VIP celebs who fell victim to the show’s vaccine mandate.
Strictly Come Dancing 2021: will Tom Fletcher return after positive Covid test - are the dancers vaccinated?
One day after the first live show, it was announced by the BBC that the McFly musician and his professional dancing partner Amy Dowden had both tested positive for Covid-19
… Have all the dancers been vaccinated?
The news of Fletcher and Dowden testing positive for Covid-19 comes after unconfirmed reports that some of the dancers have not been vaccinated, however there is no suggestion that Fletcher and Dowden are among those numbers.
Present day:
McFly’s Tom Fletcher details unexpected A&E visit after shock ‘flare up’
Tom Fletcher has revealed that he had an unexpected visit to A&E earlier this week after he woke up looking like he had been “smashed in the fact”.
The McFly singer lives with a rare autoimmune condition called uveitis, which causes inflammation on the inside part of your eye.
In a selfie shared on Monday (31 March), one of Fletcher’s eyes appeared swollen and droopy.
He wrote: “My autoimmune thing flared up out of nowhere last night (Sunday). Woke up feeling (and looking) like I'd been smashed in the face! This is after it had calmed down and I could see again.”
Denial, work pressure, a culture of lies, cover-ups and blackmail, a lack of critical thinking skills, a lack of reading case reports & papers, or they’ve been going around with their heads in a bucket for the last five years?
Charity urges Government to consider needs of teenagers in national cancer plan
… There should also be support and training for GPs and other health professionals to improve awareness of the signs and symptoms of cancer in younger people, it said.
It comes after a 2023 Cancer Patient Experience Survey found almost half (48%) of teenagers and young adults diagnosed with cancer had to see their GP three or more times before being referred to specialists.
Mariam Sohail was diagnosed with Hodgkin lymphoma at the age of 18.
It took nine months from when she first noticed symptoms to start treatment, and she visited her family doctor multiple times.
Now 23, Ms Sohail said: “If I could say one thing to Wes Streeting it would be to have young people taken more seriously and have their concerns listened to.”
During the “campaign”:
Present day:
I wish this were fake news, a sick April Fool’s joke.
Hospital's response as TEN maternity nurses develop brain tumors
A Massachusetts maternity ward has seen a spike in nurses diagnosed with brain tumors - as staff fear conditions are making them sick.
Workers at Newton-Wellesley Hospital have been struck with different types of brain tumors over the years.
One claimed as many as ten nurses on the same floor - including herself - had been diagnosed.
While some have been benign and some cancerous, she believed that the diagnoses were serious cause for concern for the site.
The nurse told WBZ-TV: 'It's getting to the point where the number just increases, and you start saying am I crazy thinking this. This can't just be a coincidence.'
She told the outlet three of them have had surgery, but believed the hospital has not been supportive enough.
'We want reassurance because this has not been a reassuring past few months for a lot of the staff members,' she said.
'We want to feel safe, the same way we want to make our patients feel safe.'
One nurse claimed that as many as ten nurses on the same floor, including herself, received a brain tumor diagnosis. This can't just be a coincidence,' she said
The hospital claimed that there were 'no environmental risk' after conducting an investigation since December
Concerns had been growing in the department among nurses, as the number of their colleagues struck with the diagnosis only increased.
'You're going into work every day with that feeling in your gut, and it's a lousy feeling,' she told the outlet.
The hospital, however, gave a shocking response claiming there were 'no environmental risk' after investigating since December.
In a statement the hospital said: 'After we became aware of reported brain tumors in individuals who currently or previously had worked in the same area of the hospital, we conducted an extensive investigation in collaboration with the Department of Occupational Health and Safety, Newton-Wellesley Safety Officer, radiation and pharmaceutical safety offices, and external environmental consultants.'
The hospital told the outlet it had interviewed ten nurses, five of which were said to have different types of brain tumors.
'Every staff member who came forward was given the opportunity to be interview by the Occupational Health and Safety team to evaluate each diagnosis in the context of their individual medical history and risk factors.
… Paula Ward of the Massachusetts Nurse Association told the outlet:' I think the concern is [that] we don't know what it is, and nurses are scared, they're worried, and they want to make sure they're not working in an unsafe place.'
Of course, there is no “environmental risk”, but they don’t use the V-word.
Do we really need to spell it out?
After spending the last few months writing about saRNA and mRNA vaccine-linked immunosuppression, HERVs and glioblastoma, it unfortunately comes as no surprise.
Out of interest, I went to Google Trends to track 5-year searches for "Brain cancer".
Searches mirror a serious and concerning increase in case reports, and probably reflect a minimum latency of 4-5 years after administration of The Thing™.
It gets worse. These are likely just the earliest cases, as the bell-curve steepens:
Back in March ‘22 I walked through an analysis of the metabolic changes to brain glial cells induced by BNT162b2 which means that brain tumours are more likely to progress: “Decoding COVID-19 mRNA Vaccine Immunometabolism in Central Nervous System: human brain normal glial and glioma cells by Raman imaging”
“Our results from Fig. 10 show that apoptosis is reduced upon mRNA vaccine for astrocytoma and glioblastoma which indicate decreased ability to fight against cancer development by programmed cell death.”
More:
5-10 cases in one ward? I don’t know what sigma “black swan” event that would have to be if this were happening by chance alone.
Statistically, if you put all the staff from all the Boston hospitals together, you should struggle to find even one case. And even then, glioblastoma used to mostly affect the elderly:
There is a long history of them gaslighting you about glioblastoma, and cancer risk in general.
For example, the arrogance of saying it cannot occur less than five years after exposure.
What difference does it make, even if it only took, say, 4 years to become symptomatic and positively diagnosed? It takes as long as it takes, we are all different.
One of my early Substacks discussed how tumours in transplanted organs grew extremely quickly in patients on first generation anti-rejection drugs. They were detected only months later, despite the organ being accepted as healthy and cancer-free.
The following question was answered by an expert in the appropriate field:
Q
Could working at Hanford in Buildings 300 and 303 (where the bombs were made) from January 1944 to August 1945, and then working at the Berkeley Radiation Lab (now Lawrence Berkeley National Laboratory [LBNL], where radiation experiments were carried out) from November 1945 to June 1948 cause a glioblastoma?
I am asking because my grandfather worked at Hanford and LBNL from 1944 to 1948. He died of a glioblastoma. His grandchildren have applied for compensation from the Energy Employees Occupational Illness Compensation Program Act (EEOICPA) fund. However, he died three and a half weeks too soon. In order to qualify for the compensation, there has to be a five-year latent period. Had he lived another month, it would have been five years between the start date of his work at Hanford and the date of his death, and we would have qualified for compensation.
Here is why I am writing: If one has a glioblastoma, which is a fast-growing tumor, the estimated life expectancy is less than a year. So, if one develops a glioblastoma from exposure to radiation, then it is not likely the person would last out the fund's required five-year latent period. If you can shed any light on this, we would be grateful.
A
First, the answer to your question of whether radiation could cause a glioblastoma is clearly yes. However, to determine whether to provide compensation, the U.S. Department of Labor (DOL) must answer a different question, in accordance with the provisions of EEOICPA. The DOL must use probability of causation (PC); that is, they must determine the likelihood that the worker's cancer was caused by exposure to radiation during employment. You can find a discussion of PC on the Centers for Disease Control and Prevention (CDC) website.
If the PC is 50% or greater (if the cancer was at least as likely as not to have been caused by exposure during covered employment), the energy worker (or their survivors) is eligible for compensation from DOL: $150,000, plus medical benefits for surviving energy workers for their cancer treatment.
An important part of determining the PC is latency. It takes time (the latent period) for a cancer to appear after the radiation exposure occurs. A latent period of decades may elapse between radiation exposure and the detection of cancer. The latent period for most cancers, including glioblastoma, is much longer than five years. The shortest latent periods, about five years, are for leukemia and thyroid cancer.
Nevertheless, the EEOICPA established its own rules about latency for different kinds of cancers. You can view those rules on the CDC website. As this web page says, "… a covered employee … [may] qualify for compensation [for primary cancer of the brain] … provided onset was at least five years after first exposure."
Apparently, even after giving the benefit of the doubt regarding latency for radiation-induced glioblastoma, the DOL was unable to award your family compensation under the provisions of the EEOICPA. It appears that the reason the claim could not be granted compensation is because the latency period of at least five years between exposure and the time of development (diagnosis) of the cancer was not met.
You can appeal the decision to the DOL Final Adjudication Branch. For a brief description of the entire EEOICPA claim process, see the DOL brochure.
Bob Cherry, CHP, PhD
I agree his job may be to blame for his brain cancer, but not for the same reason.
Father-of-five told he has months left to live - and his job could be to blame
A decorated RAF helicopter pilot has been diagnosed with terminal brain cancer that could have been caused by fumes from his aircraft.
Despite this, Philip “Pip” Harding has praised the "potentially life-saving" support he has received from the force.
Welcome to “Autoimmune City”:
“Study of 9 Million Reveals Crisis of Brain Damage Among Covid-Vaccinated”
"The researchers found alarming surges in several conditions, including ischemic stroke, hemorrhagic stroke, transient ischemic attack, myelitis, myasthenia gravis, Alzheimer’s disease, cognitive impairment, depression, anxiety, and sleep disorders."
This explains a great deal - ❗
One of the largest studies to date has revealed an alarming crisis of neurological and psychiatric damage among people who received Covid mRNA “vaccines.”
The explosive study, involving almost 9 million participants, has exposed a devasted surge in deadly disorders and long-term damage.
According to the peer-reviewed study, just one dose of an mRNA injection puts recipients at risk of suffering from several severe neurological diseases.
More: https://slaynews.com/news/study-9-million-reveals-crisis-brain-damage-among-covid-vaccinated/
From: “Why NIH Laboratories Face Supply Shortages and Institutional Challenges at the CDC”.
… Institutional Struggles at the CDC: Policy Interference and Internal Discord
Simultaneously, the CDC has encountered growing internal unrest, exemplified by a controversial April Fool’s memo circulated among staff on April 1, 2025. The memo falsely announced the reinstatement of previously restricted scientific terms, including “diversity,” “equity,” and “climate change.” While intended as a joke, the incident highlighted underlying discontent among CDC personnel who have faced increasing constraints on scientific communication.
“This prank, while inappropriate, reflects the broader frustration within the agency,” noted a former CDC official. “The administration’s continuous interference in public health messaging has created an environment of uncertainty and demoralization among scientists.”
More: https://researcherdaily.com/p/why-nih-laboratories-face-supply
Stop tittering at the back there, it’s not funny.
Calley says the quiet bit out loud, then lobs in a few sh!t grenades for dessert:
RFK Jr.'s Advisor Torches Anti-MAHA Lobbyists: "Insane To Think More Bureaucrats = Better Health"
Calley Means, co-founder of the Truemed telehealth platform and a special government employee at the Department of Health and Human Services advising Robert F. Kennedy Jr., defended efforts to eliminate waste and fraud within federal health agencies.
During a tense exchange at the Politico Health Care Summit on Wednesday, Means criticized existing federal health authorities as an "utter failure," prompting one healthcare lobbyist in the crowd to shout, "That's not true!" Means then proceeded on a warpath with stats, shutting up the room of anti-MAHA lobbyists.
Here's the exchange:
Calley: "Those scientists fundamentally have overseen a record of utter failure."
Lobbyist: "That's not true!"
Calley: "Oh, that's not true?"
"Has there been one single chronic disease medication in modern American history that has lowered rates of the chronic disease?"
"Is it appropriate that the American Academy of Pediatrics right now, which is 90% funded by pharma, is pushing Ozempic on six year olds?"
"The lobbyists in this room do not have the humility to admit that we have gone completely wrong."
"The lobbyists in this room laughing when we have the sickest children in the developed world."
Its not just glioblastoma:
With that in mind, unbelievably, your government are still poisoning and killing your children - democide, under a never-ending Emergency Use Authorisation (EUA).
RFK Jr. has called for new safety studies.
Whatever it takes, this plörre just needs to be pulled ASAP.
Dr. Mary Talley Bowden left Tucker Carlson visibly shaken after dropping a chilling COVID vaccine statistic that’s impacting millions of children right now.
… Before Tucker became visibly disturbed, Dr. Bowden pointed to data from the CDC’s VAERS system, explaining that over 38,000 deaths have been reported following the rollout of the so-called COVID-19 vaccines.
She said that under normal circumstances, such numbers would’ve prompted the FDA to pull the shots.
Instead, they pushed forward, adding the COVID vaccine to the routine childhood schedule, with the expectation that babies receive three doses by just nine months of age.
She added that the shots are still under Emergency Use Authorization (EUA) for children under 12—not fully FDA approved—and yet they remain on the official vaccine schedule.
… Tucker was horrified when Dr. Bowden mentioned a disturbing fact: “According to the CDC, 9 million American children have gotten the latest version of these COVID shots,” she said.
Clearly caught off guard, Carlson asked, “Actually?”
“Yes,” Bowden confirmed.
“Still?” he pressed.
“Yes. Yes. 9 million [kids]—12% [of US children have been injected].”
Tucker, in disbelief, asked, “Wait, this is going on right now?”
“Yes,” Bowden replied.
“I think we voted against this,” Tucker said.
“Yeah,” Bowden confirmed.
“Correct?” Tucker stressed.
“I don’t know,” Dr. Bowden answered.
“You’re very diplomatic, but I’m just stunned to learn that that’s happening right now,” Tucker exclaimed.
“Could this be shut down?” he asked.
“It should have been shut down a long time ago,” Dr. Bowden answered. “And you know, what’s the—”
Tucker interrupted: “9 million babies have had COVID shots?”
“Yeah. Well, children. Minors,” Dr. Bowden clarified.
Tucker’s reaction at the end says it all:
Concluding remarks
In summary, natural autoantibodies also play as large a part in neurological disease progression and symptomatology as pathogenic aAbs. Pathogenic aAbs may be useful too. And low levels of aAbs may be as harmful as elevated levels, as healthy immune homeostasis relies on optimum levels of both, in balance. Plus, we have an immunculus which includes a complex network of antiidiotypic antibodies with regulatory roles.
Their findings showed that neural, organ, or non-organ antigens lead to abnormal targeting by both pathogenic, but mostly natural autoantibodies, and that disrupted immunostasis correlates with disease symptom scores.
These levels also vary according to tissue, nerve or organ type, and whether the individual has just sustained an injury or infection.
Molecular mimicry by both viral and vaccinal epitopes may be sufficient to trigger autoimmune dysregulation, augmented by regulatory T-cell dysfunction24. This continues even after the primary antigen (e.g. Spike, LNPs) has been cleared, contributing to the spectrum of Long COVID and long vaccine cases with ME/CFS and FMS-like symptoms.
The more you study it, the more complicated the picture becomes. I’ve certainly had to adjust my line of thinking.
I hope this Substack goes some way towards changing attitudes towards sufferers, and helps them to move closer to getting a more accurate diagnosis, with an improved prognosis as treatments become more effective.
I do fear, however, that the NHS isn’t geared towards this level of complexity and stealth mechanisms. This is partly due to culture, and partly due to a lack of suitable diagnostic equipment and trained personnel.
Some “specialists” are prone to a degree of arrogance, building a position they will defend to the end, rather than being open-minded and bending with the science, even if this means admitting that they may have been wrong.
Coming up, I'm planning some more objective reviews of therapeutics, such as the mystical “DMSO”.
What are the mechanisms?
Thank you for your ongoing support, and enjoy your Easter break.
Disclaimer
This site is strictly an information website reviewing research into potential therapeutic agents. It does not advertise anything, or provide medical advice, diagnosis, or treatment. This site does not promote any of these as potential treatments or offer any claims for efficacy. Its content is aimed at researchers, registered medical practitioners, nurses, or pharmacists. This content is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. Always consult a qualified health provider before introducing or stopping any medications as any possible drug interactions or effects will need to be considered.
Any extracts quoted in the previous article are for non-commercial research and educational purposes only and may be subject to copyright from their respective owners.
References
‘Definition of Sign - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/sign.
‘Definition of Condition - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/condition.
‘Definition of Symptom - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/symptom.
‘Definition of Syndrome - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/syndrome.
‘Definition of Disorder - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/disorder.
‘Definition of Disease - NCI Dictionary of Cancer Terms - NCI’. nciAppModulePage, 2 February 2011. Nciglobal,ncienterprise. https://www.cancer.gov/publications/dictionaries/cancer-terms/def/disease.
The Rehab Team - Tauranga Physiotherapy. ‘Seven Myths of Functional Neurological Disorder (FND) I The Rehab Team NZ’. Accessed 31 March 2025. https://therehabteam.co.nz/blog/functional-neurological-disorder-myths.
nhs.uk. ‘Fibromyalgia’, 20 October 2017. https://www.nhs.uk/conditions/fibromyalgia/.
McConnell, Kerrie, Neil Heron, and Nigel D. Hart. ‘Explaining a Diagnosis of Fibromyalgia in Primary Care: A Scoping Review’. BJGP Open 7, no. 4 (1 December 2023). https://doi.org/10.3399/BJGPO.2023.0033.
Clauw, Daniel, Piercarlo Sarzi-Puttini, Greta Pellegrino, and Yehuda Shoenfeld. ‘Is Fibromyalgia an Autoimmune Disorder?’ Autoimmunity Reviews, Congress of Controversies in Rheumatology and Autoimmunity (CORA), Turin, March 2023, 23, no. 1 (1 January 2024): 103424. https://doi.org/10.1016/j.autrev.2023.103424.
Zari, Ali, Elrashdy M. Redwan, Mikolaj Raszek, David Cowley, Altijana Hromić-Jahjefendić, Vladimir N. Uversky, Mark Fabrowski, Carlo Brogna, Marina Piscopo, and Alberto Rubio-Casillas. ‘Interplay between Multisystem Inflammatory Syndrome in Children, Interleukin 6, Microbiome, and Gut Barrier Integrity’. Immuno 4, no. 3 (September 2024): 226–46. https://doi.org/10.3390/immuno4030015.
Rubio-Casillas, Alberto, Mark Fabrowski, Carlo Brogna, David Cowley, Elrashdy Redwan, and Vladimir Uversky. ‘Could the Spike Protein Derived from mRNA Vaccines Negatively Impact Beneficial Bacteria in the Gut?’ COVID 4 (25 August 2024): 1368–78. https://doi.org/10.3390/covid4090097.
Carabotti, Marilia, Annunziata Scirocco, Maria Antonietta Maselli, and Carola Severi. ‘The Gut-Brain Axis: Interactions between Enteric Microbiota, Central and Enteric Nervous Systems’. Annals of Gastroenterology : Quarterly Publication of the Hellenic Society of Gastroenterology 28, no. 2 (2015): 203–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367209/.
Ronga, Alexandre, Paul Vaucher, Jörg Haasenritter, Norbert Donner-Banzhoff, Stefan Bösner, François Verdon, Thomas Bischoff, Bernard Burnand, Bernard Favrat, and Lilli Herzig. ‘Development and Validation of a Clinical Prediction Rule for Chest Wall Syndrome in Primary Care’. BMC Family Practice 13 (6 August 2012): 74. https://doi.org/10.1186/1471-2296-13-74.
Chronic Pain (Primary and Secondary) in over 16s: Assessment of All Chronic Pain and Management of Chronic Primary Pain. National Institute for Health and Care Excellence: Guidelines. London: National Institute for Health and Care Excellence (NICE), 2021. http://www.ncbi.nlm.nih.gov/books/NBK569960/.
Ryabkova, Varvara A., Natalia Y. Gavrilova, Alina A. Poletaeva, Alexander I. Pukhalenko, Irina A. Koshkina, Leonid P. Churilov, and Yehuda Shoenfeld. ‘Autoantibody Correlation Signatures in Fibromyalgia and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Association with Symptom Severity’. Biomedicines 11, no. 2 (18 January 2023): 257. https://doi.org/10.3390/biomedicines11020257.
‘Natural Autoantibody - an Overview | ScienceDirect Topics’. Accessed 1 April 2025. https://www.sciencedirect.com/topics/medicine-and-dentistry/natural-autoantibody.
‘Antiidiotypic Antibody - an Overview | ScienceDirect Topics’. Accessed 1 April 2025. https://www.sciencedirect.com/topics/neuroscience/antiidiotypic-antibody.
Poletaev, A. B. ‘The Immunological Homunculus (Immunculus) in Normal State and Pathology’. Biochemistry. Biokhimiia 67, no. 5 (May 2002): 600–608. https://doi.org/10.1023/a:1015514732179.
Disorders, Institute of Medicine (US) Forum on Neuroscience and Nervous System. ‘Overview of the Glutamatergic System’. In Glutamate-Related Biomarkers in Drug Development for Disorders of the Nervous System: Workshop Summary. National Academies Press (US), 2011. https://www.ncbi.nlm.nih.gov/books/NBK62187/.
Allen, Mary J., Sarah Sabir, and Sandeep Sharma. ‘GABA Receptor’. In StatPearls. Treasure Island (FL): StatPearls Publishing, 2025. http://www.ncbi.nlm.nih.gov/books/NBK526124/.
Strand, Natalie H., Jillian Maloney, Molly Kraus, Christopher Wie, Michal Turkiewicz, Diego A. Gomez, Olufunmilola Adeleye, and Monica W. Harbell. ‘Cannabis for the Treatment of Fibromyalgia: A Systematic Review’. Biomedicines 11, no. 6 (2 June 2023): 1621. https://doi.org/10.3390/biomedicines11061621.
Yang, Zhihui, and Kevin K.W. Wang. ‘Glial Fibrillary Acidic Protein: From Intermediate Filament Assembly and Gliosis to Neurobiomarker’. Trends in Neurosciences 38, no. 6 (June 2015): 364–74. https://doi.org/10.1016/j.tins.2015.04.003.
Dominguez-Villar, Margarita, and David A. Hafler. ‘Regulatory T Cells in Autoimmune Diseases’. Nature Immunology 19, no. 7 (July 2018): 665–73. https://doi.org/10.1038/s41590-018-0120-4.








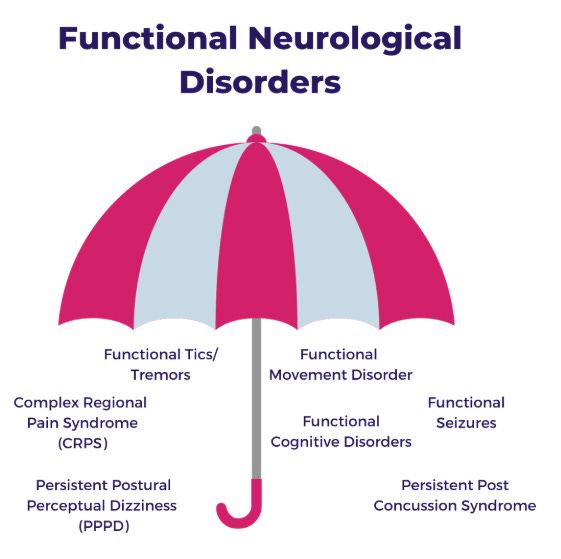
















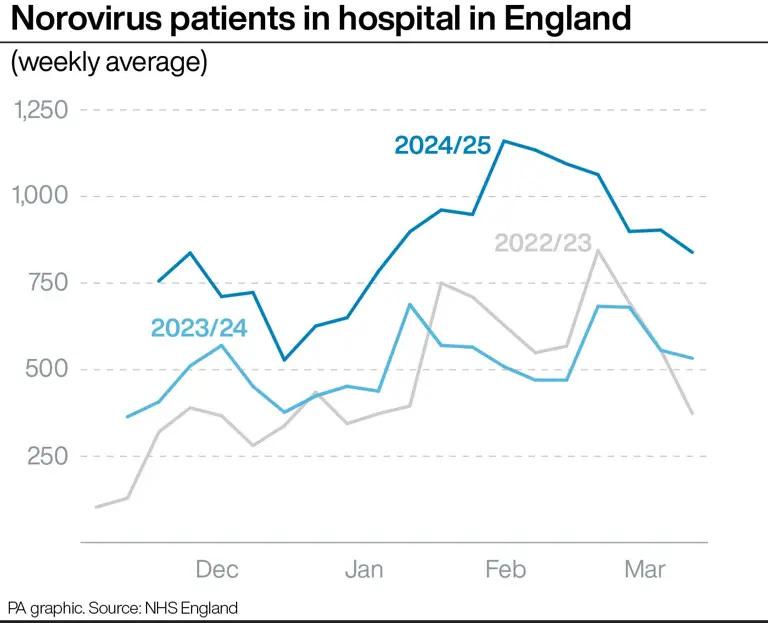
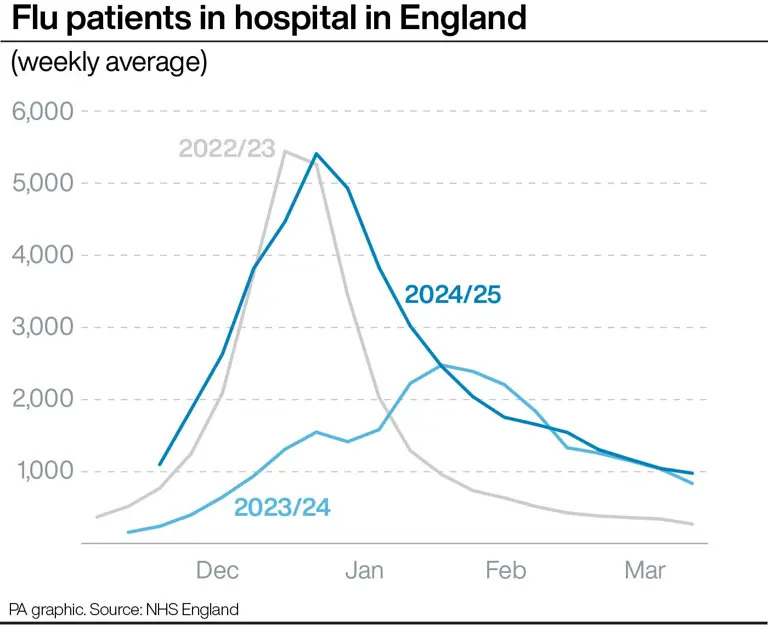





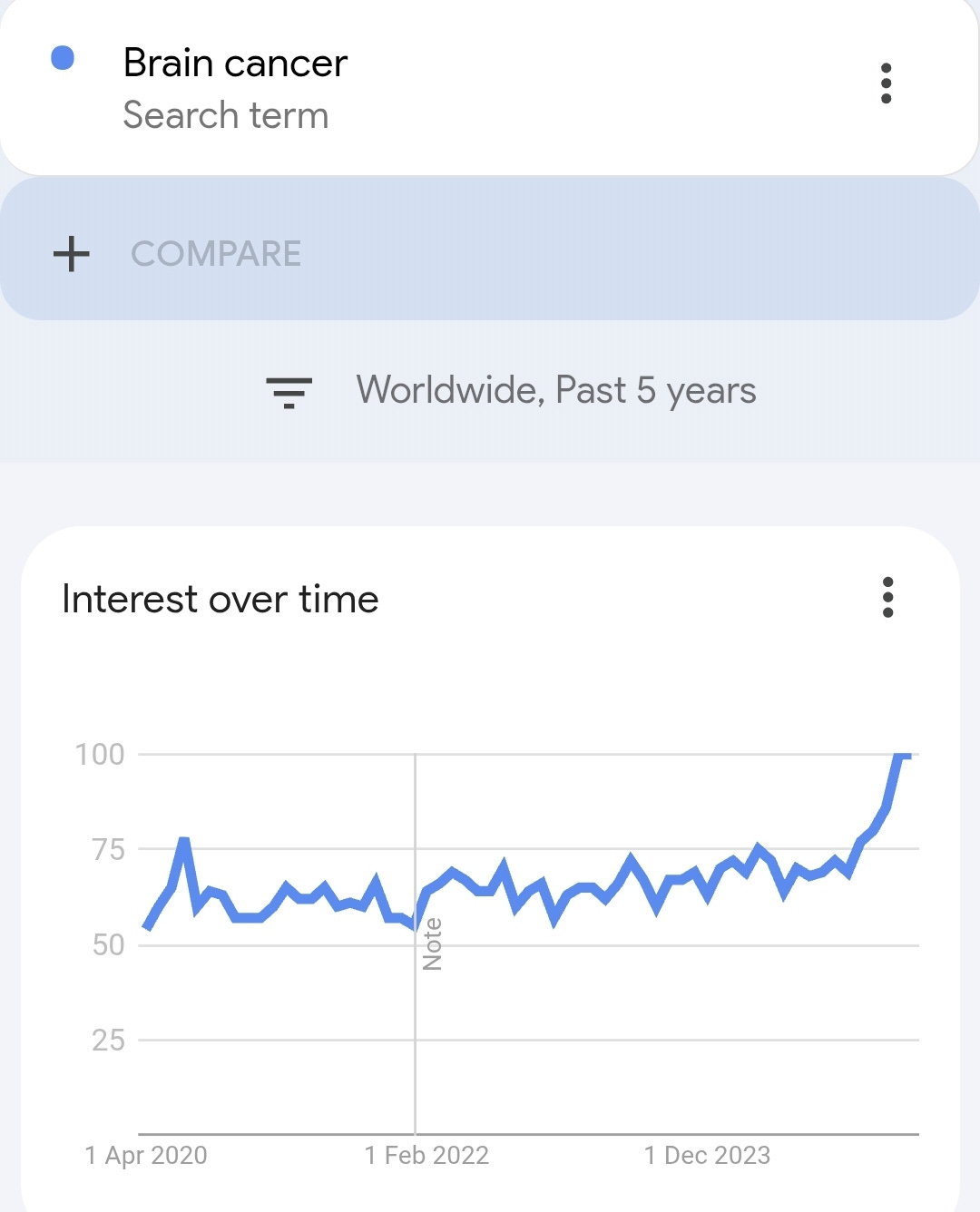




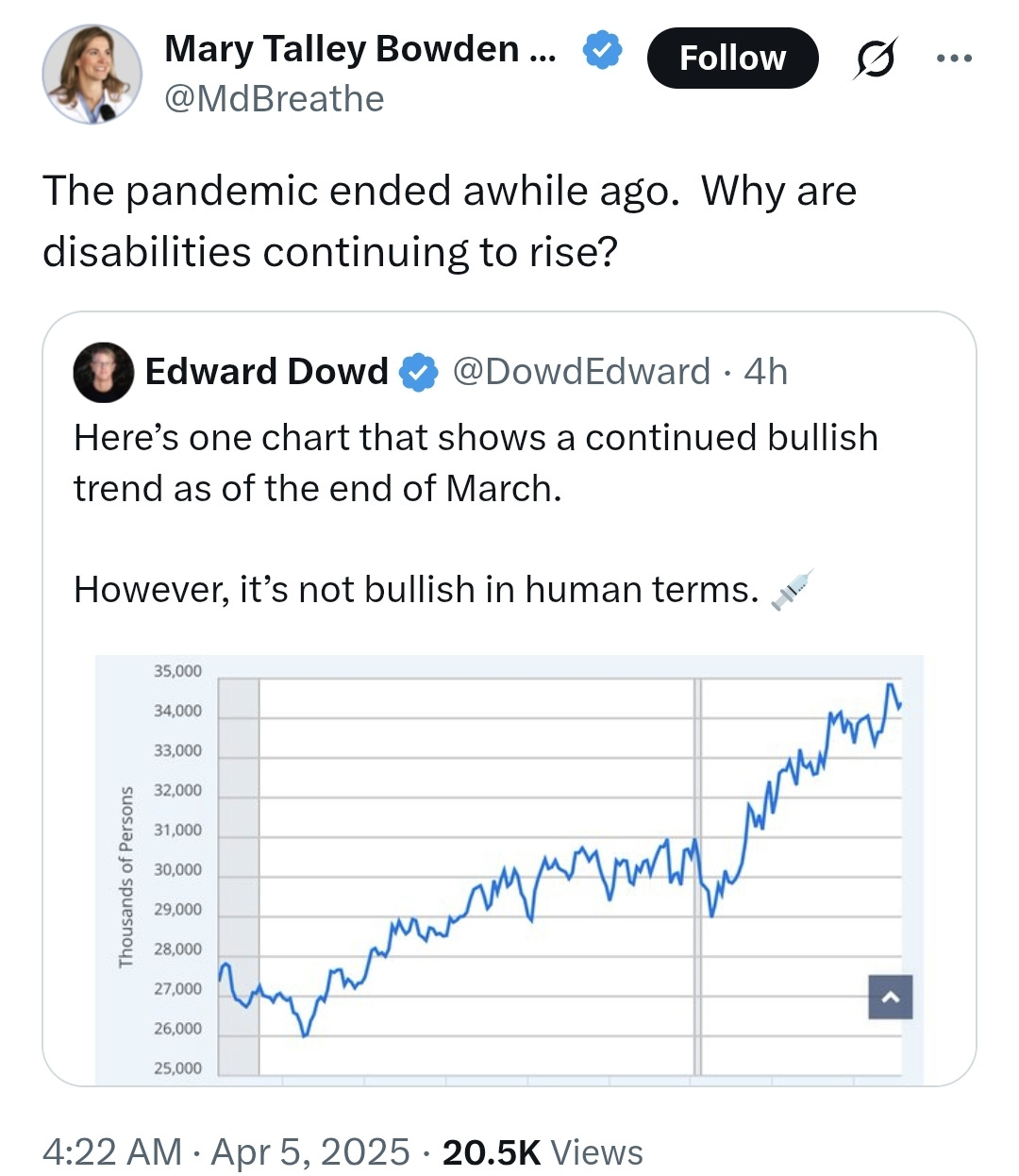
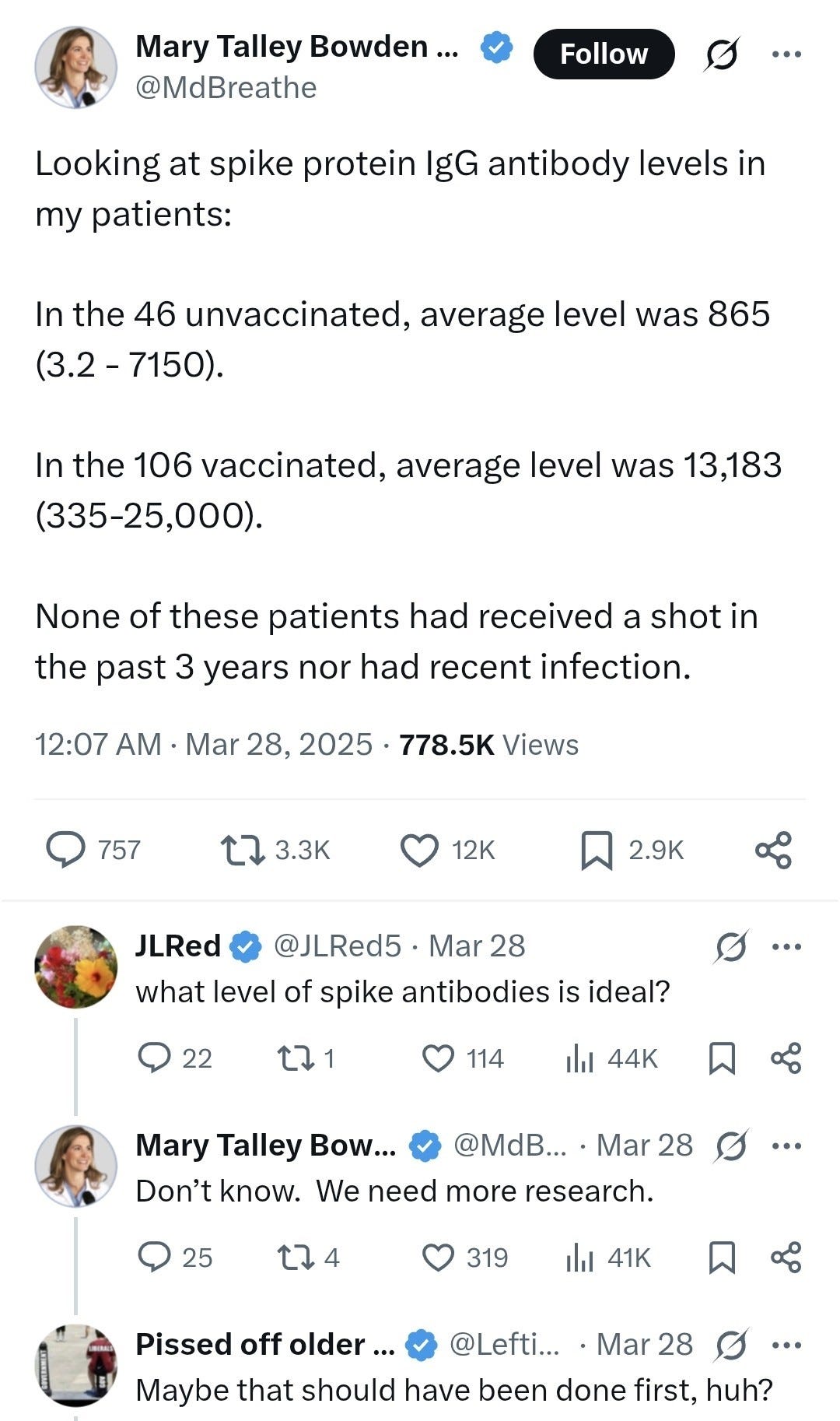

Sabine shared her related investigations:
Possible autoimmune mechanisms through COVID modRNA products
Another underlying basic damage mechanism
https://drbine.substack.com/p/mogliche-autoimmunmechanismen-durch
Follow The Science: Why Peter Marks Was Asked To Leave The FDA
... Thanks to Dr. Marks’ terrible decisions, we are left with a drug that has no proven benefit and that just killed a young patient, a vaccine that is not completely safe is being administered to children that have no significant risk of harm from the underlying infection, and an overburdened healthcare system that had to pay billions for another unproven, harmful therapy. Advocates for Dr. Marks claim that he has acted to help patients with life-threatening conditions which have no alternative treatments. But in reality, he catered to industry and hurt patients.
https://realclearwire.com/articles/2025/04/01/follow_the_science_why_peter_marks_was_asked_to_leave_the_fda_1101329.html